All published articles of this journal are available on ScienceDirect.
Large-Scale Evaluation of ureC (glmM) and SSA Conventional PCR for Rapid Direct Detection of Helicobacter pylori in Gastric Biopsies as Compared to rpoB-based Quantitative Real-Time PCR
Abstract
Background:
Conventional polymerase chain reaction (PCR)-based methods play a major role in the direct detection of H. pylori in clinical specimens, with time-saving as compared to culture-based methods. However, specificity and sensitivity vary among different varieties of these PCRs, which consequently could affect the accuracy of diagnosis of H. pylori infection. The study aimed to evaluate the utility of ureC (glmM) and SSA conventional PCR methods for rapid direct detection of H. pylori by comparing them with rpoB-based quantitative real-time PCR.
Methods:
A total of 402 non-repeated gastric biopsy specimens were subjected to DNA extraction followed by conventional ureC (glmM) and SSA PCR, and rpoB-based quantitative real-time PCR, which was used as the gold standard.
Results:
H. pylori was detected in 119 (29.6%), 126 (31.34%), and 187 (46.5%) of the tested specimens using ureC (glmM) PCR, SSA PCR, and real-time quantitative PCR, respectively. The specificity of the SSA PCR was higher than that of ureC (glmM) PCR (99.5% and 98.6%, respectively). The SSA PCR was more sensitive than the ureC (glmM), (66.8% and 62%, respectively). The diagnostic accuracy of SSA PCR (84.33%) was higher than that of ureC (glmM) PCR (81.59%).
Conclusion:
Overall, SSA PCR is more specific, sensitive, and diagnostically accurate than ureC (glmM) PCR, giving the SSA PCR assay superiority as a simple, rapid, and accurate diagnostic tool for direct detection of H. pylori in gastric tissue specimens.
1. INTRODUCTION
Helicobacter pylori (H. pylori) infection is one of the most widespread infections worldwide [1, 2]. It is considered a leading cause of chronic gastritis, peptic ulcer disease, gastric cancer, and mucosa-associated lymphoid tissue (MALT) lymphoma [3-6]. Early diagnosis of this infection is crucial to establishing an effective management plan and administering appropriate antibiotic therapy to eradicate this gastric pathogen and avoid its sequelae. H. pylori diagnostic approaches are invasive methods that are based on gastric biopsies and include urease tests, histopathology, culturing, polymerase chain reaction (PCR), or non-invasive methods that utilize the urea breath test, serological detection of antibodies, and antigen detection in stool [7-10].
PCR-based methods have great utility in the detection, genotyping, and antimicrobial resistance studies of H. pylori [11-13]. These methods include many conventional and real-time varieties that can be performed directly on gastric biopsy specimens. Overall, the main advantages of these molecular-based methods are higher sensitivity, specificity, avoidance of the time required for culture-based methods, and the ability to detect dead or inhibited bacteria resulting from the prior administration of antibiotics.
Both ureC and SSA PCRs are among the earlier conventional PCR assays used for H. pylori detection [14, 15]. The ureC PCR targets the urease C (ureC) gene, which was first wrongly believed to be associated with urease production [14], but later, it was proven to be responsible for the production of the phosphoglucosamine mutase, which is involved in the synthesis of bacterial cell walls, and renamed the glmM gene [16]. SSA PCR utilizes primers targeting the 26-kDa species-specific antigen (SSA) gene [15, 17].
An earlier study was carried out to compare conventional PCR methods used for the detection of H. pylori in gastric tissues, including these two PCRs, and demonstrated higher sensitivity and specificity for ureC PCR over SSA PCR [18]. However, this study used a limited number (50 cases) of gastric biopsy specimens and took the culture method as the gold standard for comparison, which can be biased by false negative cases resulting from dead or inhibited bacteria. The current study reevaluated and compared these two PCR methods in the presence of different test conditions either tested population or test methodology, to investigate if these differences could affect the sensitivity, specificity and diagnostic accuracy of these PCR methods. The study compared ureC (glmM) PCR and SSA PCR on a wide-scale using a large number of gastric biopsies (exceeding 400 specimens) obtained from dyspeptic Saudi patients and taking rpoB real-time PCR, which targets the RNA polymerase beta-subunit (rpoB) gene, as the gold standard to avoid false negative results of culture. The principal aim was to evaluate the diagnostic value and utility of these simple PCR approaches in the direct detection of H. pylori in gastric biopsies, aiming at a rapid and accurate diagnosis of H. pylori infection, which will serve to establish appropriate treatment plans for this common pathogen.
2. MATERIALS AND METHODS
2.1. Study Population and Clinical Specimens
The study included 404 Saudi patients attending gastroenterology clinics at general hospitals in the Jazan region of Saudi Arabia. All patients who participated in this study had dyspeptic symptoms. The study tested 402 non-repeated gastric biopsies obtained from 402 patients of the study population (one biopsy from each patient), while the remaining two biopsy specimen materials obtained from the remaining two patients were insufficient for further processing. Upper gastrointestinal endoscopy was performed to obtain the specimens.
2.2. DNA Extraction
The biopsy specimens were subjected to DNA extraction using a DNeasy blood and tissue kit (Qiagen) (Cat. No. 69504) according to the manufacturer’s instructions.
2.3. Conventional PCR
Each specimen was examined by both ureC (glmM) PCR and SSA PCR. In ureC (glmM) PCR, the H. pylori DNA was amplified by targeting the ureC (glmM) gene, which is common for all H. pylori strains, using a forward primer (5՛-AAG CTT TTA GGG GTG TTA GGG GTT T-3՛) and a reverse primer (5՛-AAG CTT ACT TTC TAA CAC TAA CGC-3՛) (TIB MOLBIOL, Germany) [14]. In SSA PCR, the specimens were tested for the presence of species-specific DNA sequences coding for a protein antigen of 26 kDa molecular weight, which is present in all H. pylori strains, using the forward primer (5՛-TGG CGT GTC TAT TGA CAG CGA GC-3՛) and the reverse primer (5՛-CCT GCT GGG CAT ACT TCA CCA TG-3՛) (TIB MOLBIOL, Germany) [15]. In both PCR methods, reactions were carried out in volumes of 50 µl containing 2.5 U of FastStart Taq DNA polymerase (Roche, Germany), reaction buffer (50 mM KCl, 10 mM Tris-HCl [pH 9.0], 1.5 mM MgCl2, deoxynucleoside triphosphate mix [0.2 mM each of dATP, dCTP, dGTP, and dTTP] (Roche, Germany), 0.4 µM of each primer, 7 µl of template DNA, completed to a 50 µl volume with sterile RNase/DNase-free water. Positive and negative controls were included in each PCR run. DNA extracted from a gastric biopsy specimen of a well-known H. pylori-positive patient was used as a positive control, while the negative control reaction contained RNase/DNase-free water instead of genomic DNA. PCR reactions were performed under the cycling conditions described previously [19, 20] with some modifications as follows: initial denaturation for 10 min at 94 oC, followed by 35 cycles of denaturation for 2 min at 94 oC, annealing for 2 min at 55 oC (for ureC (glmM) PCR), and 57 oC (for SSA PCR), and extension for 2 min at 72 oC, followed by a final extension for 10 min at 72 oC. The resulting products were separated in 2% agarose gels and 1x Tris-acetate-EDTA buffer, and images were captured after staining with ethidium bromide.
2.4. Real-Time PCR
Quantitative real-time PCR for the detection of H. pylori was used as the gold standard in this study. It was performed for all extracted DNA samples by targeting the RNA polymerase beta-subunit (rpoB) gene of H. pylori using the primer-probe based “genesig Quantification of Helicobacter pylori advanced kit” (PrimerDesign Ltd. Southampton, United Kingdom) as described previously [12].
2.5. Statistical Analyses
Sensitivity, specificity, positive predictive value, negative predictive value, and diagnostic accuracy, and their 95% CI were determined for each of the tested conventional PCRs in reference to the quantitative real-time PCR, which was taken as the gold standard. Analyses were conducted using SPSS software.
3. RESULTS
A total of 402 gastric biopsy specimens were tested for the presence of H. pylori using ureC (glmM) PCR, SSA PCR, and rpoB quantitative real-time PCR, which was considered the gold standard test.
3.1. Quantitative Real-Time PCR
The quantitative real-time PCR assay detected H. pylori in 187 (46.5%) of the total tested specimens, while 215 (53.5%) cases were negative for H. pylori (Table 1).
3.2. ureC (glmM) PCR
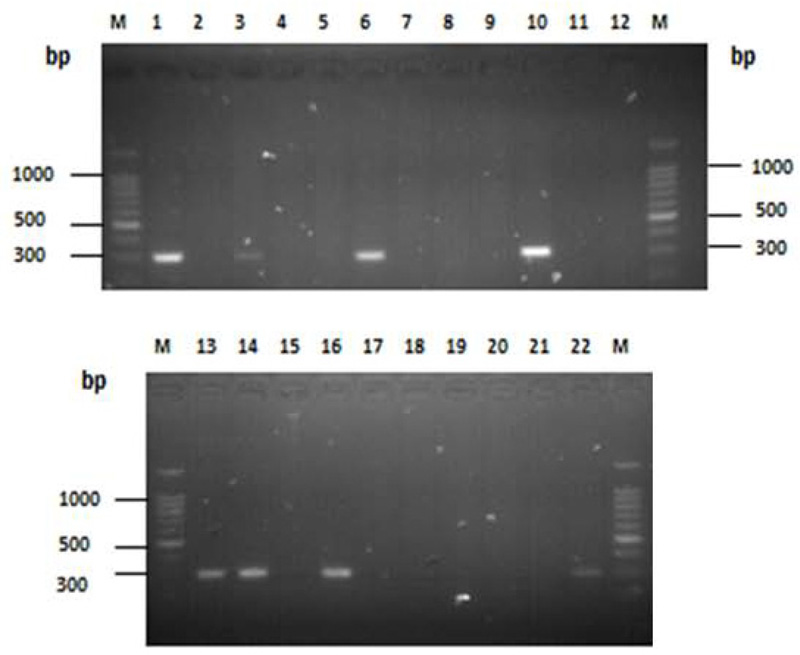
The ureC (glmM) PCR resulted in an amplified product of approximately 294 bp in size Fig. (1). Of 402 specimens, 119 (29.6%) were H. pylori-positive, while the remaining 283 (70.4%) were H. pylori-negative (Table 1).
| rpoB-based quantitative real-time PCR | Sensitivity | Specificity | Positive Predictive Value | Negative Predictive Value | Diagnostic Accuracy | ||||
|---|---|---|---|---|---|---|---|---|---|
|
+ve (n)* |
-ve (n) |
Total (n) |
|||||||
| ureC (glmM) PCR | +ve | 116 | 3 | 119 | 62% (54.9-68.68) |
98.6% (95.98-99.52) |
97.5% (92.85-99.14) |
74.9% (69.55-79.61) |
81.59% (77.51-85.08) |
| -ve | 71 | 212 | 283 | ||||||
| Total | 187 | 215 | 402 | ||||||
| SSA PCR | +ve | 125 | 1 | 126 | 66.8% (59.82-73.19) |
99.5% (97.41-99.92) |
99.2% (95.64-99.86) |
77.5% (72.25-82.06) |
84.33% (80.45-87.56) |
| -ve | 62 | 214 | 276 | ||||||
| Total | 187 | 215 | 402 | ||||||
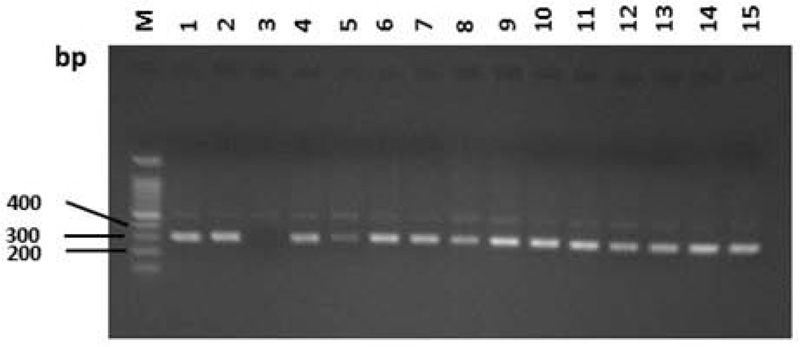
3.3. SSA PCR
From the overall tested DNA samples, 126 (31.34%) were positive for the presence of SSA sequence, which gave the PCR amplified product of 298 bp in size (Table 1 and Fig. 2).
A comparison of both conventional PCRs with quantitative real-time PCR is presented in (Table 1). The SSA PCR was more sensitive than the ureC (glmM) (66.8% and 62%, respectively). Although both types of PCR showed high specificity, the specificity of the SSA PCR was higher than that of ureC (glmM) PCR (99.5% and 98.6%, respectively). Overall, the diagnostic accuracy of SSA PCR was higher than that of ureC (glmM) PCR (84.33% and 81.59%, respectively).
4. DISCUSSION
Routine conventional PCR methods play a major role in the direct detection of H. pylori in clinical specimens, with the advantage of saving time, compared to culture-based methods. However, the different varieties of these routine PCRs differ in specificity and sensitivity, which could affect the accuracy of the diagnosis of H. pylori infection.
This study compared two types of routine PCRs, namely ureC (glmM) PCR and SSA PCR, with the gold standard rpoB gene-based quantitative real-time PCR assay. The aim of these comparisons was to investigate the diagnostic accuracies of these conventional PCRs in the direct detection of H. pylori in gastric biopsies obtained from dyspeptic patients under test conditions different from previous studies, a namely large number of tested clinical specimens, patients from different geographic region, different DNA extraction methodology, and different gold standard.
The quantitative real-time PCR assay used in our study was taken as the gold standard because it is highly specific and sensitive for the detection of H. pylori [21]. It is highly specific because it targets the RNA polymerase beta-subunit (rpoB) gene of H. pylori using a primer-probe-based approach (both the primer and probe provided with the kit are highly specific for H. pylori). As stated by the manufacturer, this kit can detect all H. pylori strains as the primers represent 100% homology with over 95% of the NCBI database reference sequences available at the time of kit design. Moreover, it is highly sensitive; by generating a standard curve using the positive control H. pylori DNA template provided with the kit, we found that the detection limit was two copies of the target gene of H. pylori per µl of the tested DNA (data not shown). Consequently, the use of such real-time PCR assay provided an advantage over the culture method by avoiding false negative results from dead or inhibited bacteria present in tested gastric biopsies.
Both tested conventional PCR methods exhibited high specificity (approximately 100%, with less than 1% difference, 98.6% and 99.5% for ureC (glmM) and SSA PCR, respectively). These findings are in complete concordance with Bickley et al. [14] and Lage et al. [19] who confirmed the specificity of ureC (glmM) PCR because the primers used did not amplify any DNA extracted from variable bacterial species other than H. pylori, including other members of the Helicobacter genus. This could be explained by the high specificity of the primers used and conservation of their target gene sequences in most H. pylori strains [14], which enables these primers to anneal specifically to their target genes.
Our results also concur with O’Toole et al. [17] who demonstrated, after sophisticated work for isolation and characterization of this specific antigen protein by determining the DNA sequence of its gene fragment, that the species-specific antigen (SSA) is unique for all H. pylori strains. These data were later used to design specific primers targeting this genomic sequence for utilization in PCR assays, which proved to be highly specific for H. pylori detection [15, 20]. Moreover, because of the universal presence of SSA in all H. pylori strains, it was used as a marker for the presence of H. pylori, acting as a positive control. Consequently, the SSA PCR assay was utilized in some studies to check the samples that were negative for H. pylori after other PCR methods used in genotyping studies [20, 22].
Despite the high specificity of both PCRs, very few false-positive results have been recorded, with three cases and one case, for ureC (glmM) and SSA PCR, respectively. This could be due to DNA cross-contamination during biopsy specimen processing, DNA extraction, or the PCR procedure itself [14].
Our results revealed 62% and 66.8% sensitivities for ureC (glmM) PCR and SSA PCR, respectively. Similarly, other studies have demonstrated variable sensitivities for both types of PCR. Lu et al. [18] found equal sensitivities for both ureC (glmM) and SSA PCR, with a detection limit equal to approximately 50 H. pylori bacterial organisms. By increasing cycle step durations to 2 min, Lage et al. [19] improved the sensitivity of ureC (glmM) PCR to a detection limit of approximately two genomes of H. pylori. Compared to our quantitative real-time PCR gold standard, the false-negative results were clearly high, with 71 and 62 cases, for ureC (glmM) PCR and SSA PCR, respectively. Such false results can be explained by occasional sequence polymorphisms that may result from point mutations in target gene sequences [23, 24] leading to the inability of primers to anneal to their targets, or the presence of PCR inhibitors, mostly from the gastric tissue specimens [25], or low or bad quality fragmented or sheared DNA.
Overall, our results, using quantitative real-time PCR as the gold standard, revealed higher specificity, sensitivity, predictive values, and diagnostic accuracy of SSA PCR over ureC (glmM) PCR. This contrasts with the findings of Lu et al. [18], who found that ureC (glmM) PCR was equally sensitive to, but more specific than, SSA PCR, taking the culture method as the gold standard. They attributed the lower specificity of the SSA PCR method to its amplification of 10 culture-negative samples. Therefore, considering the culture method as the gold standard may be the cause behind the lower specificity of SSA PCR reported in this study, as these SSA PCR-positive 10 samples may be true positive, but the culture method could not detect them. Although the culture method is considered the most specific diagnostic tool, its sensitivity to H. pylori may be low in the presence of dead or inhibited bacteria in the biopsy specimens as a result of the use of antimicrobials or improper specimen transport. The differences observed between our findings and those of others could be attributed to differences in study conditions, including the number of specimens tested, demographic and social characters of the study population, specimen preparation and processing, DNA extraction methodology, the assigned gold standard, and PCR conditions (including differences in thermocycler ramp rates).
CONCLUSION
The study reevaluated the utility of SSA PCR and ureC (glmM) PCR in the diagnosis of H. pylori infection with modification in some study conditions, including enrollment of a large number of study population from a different geographic region, different gold standard and different DNA extraction methodology. Based on our large number of tested gastric biopsies (402 non-repeated specimens) and our highly specific and sensitive gold standard (rpoB-based quantitative real-time PCR), we conclude that SSA PCR is more specific, sensitive, and diagnostically accurate than the ureC (glmM) PCR, and that the SSA PCR assay is a simple, rapid, and accurate diagnostic tool for the direct detection of H. pylori in gastric tissue specimens.
LIST OF ABBREVIATIONS
| PCR | = Polymerase Chain Reaction |
| MALT | = Mucosa-associated Lymphoid Tissue |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The study was approved by the research ethics committee at the faculty of Medicine - Jazan University with reference number (Ref: FMRERC-2012).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national), and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed written consent was obtained from each patient participating in the study.
AVAILABILITY OF DATA AND MATERIALS
The datasets generated and/or analyzed during the study are available from the corresponding author on reasonable request.
FUNDING
This research was funded by the King Abdulaziz City for Science and Technology (KACST) (Grant number: ARP-47-32).
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
We express our deep appreciation to King Abdulaziz City for Science and Technology (KACST) for the financial and technical support of this research. We would like to extend our special thanks to our colleagues in gastrointestinal units at general hospitals in the Jazan region for their support. The technical assistance provided by Mohammed Awad and Ahmed Saad is greatly appreciated.


