All published articles of this journal are available on ScienceDirect.
Factors Associated with Poor Uptake of HIV Counselling and Testing amongst Adult Men at Health Facilities in Rustenburg Sub-district, South Africa
Abstract
Background:
HIV counselling and testing (HCT) is one of the ways of reducing the prevalence of HIV infection and ensuring that infected individuals receive appropriate care. Unfortunately, the uptake of HCT amongst males, aged 15 to 49 years remains low.
Aim:
The aim of the study was to identify factors influencing low uptake of HCT amongst males between the ages of 15 and 49 in the health care facilities of Rustenburg.
Methods:
It is a cross-sectional descriptive study among 15- and 49-years males who visited 19 health facilities within Rustenburg using a self-administered questionnaire.
Results:
Four hundred and forty (440) males (15-49 years) took part in the study with a response rate of 98%. Of this total, 39 (9%) had never been tested for HIV. Most (79.1%) of participants undertook HIV testing for health reasons. The results indicated that differences in age (males aged between 40 and 49 years) and employment status (employed men) translated to differences in the likelihood of one being tested and these two variables (age and employment status) were associated with knowledge as a factor in the acceptance and usage of HCT services. Knowledge about HCT services was significantly associated with acceptability and usage of HCT services (P<0.05).
Conclusion:
Participants aged between 15 and 29 years were less likely to undergo HIV testing than other age groups. There is a need to encourage young people to undertake HIV testing since they are the most vulnerable age group.
1. INTRODUCTION
According to the latest HIV statistics, there were 39 million people living with HIV in 2022, and 1.3 million people were newly infected with HIV [1]. This is still a long way from the ambitious target to end AIDS by 2030, which was adopted by UN member states in 2021, on the signing of the Political Declaration on HIV and AIDS: Ending Inequalities and Getting on Track to End AIDS by 2030 [2]. The sub-Saharan African region continue to share a significant portion of the global burden of HIV with women and young girls accounting for 63% of all new infections in the region [3]. South Africa remains the epicentre of the global pandemic with an estimated 8.45 million people living with HIV by the end of 2022 [4], and almost a fourth of women in their reproductive ages (15–49 years) are living with HIV. Data from a national population based survey is showing an upward trend in the engagement of in age-disparate relationships (defined as having a sexual partner 5+ years different from oneself) among females since 2005 and a steady rise since 2008 in multiple sexual partners (MSP) as appose to a decline that was noted in self-reported MSPs among males from 2012 to 2017. However, men are more likely to engage in early sexual debut (first sex before the age of 15 years) and are less likely to have tested for HIV compared to their female counterparts [5]. It is important that we highlight the factors that contribute to men not testing for HIV because current data indicates that this might have a negative impact on the health of both men and women [6].
There are increasing calls for health systems and particularly HIV programmes, to be intentional about their efforts to include and engage men in interventions to challenge harmful gender norms that will enhance both men’s and women’s health [6, 7]. A report which exclusively looked at men and HIV in South Africa [7] raised the concern that men might be left out of the HIV response globally, but particularly in South Africa, where the HIV epidemic is concentrated around women. This “blind spot” as it is quoted by the UNAIDS report is totally understandable given the high incidence of HIV among women and young girls, however, this is at the expense of men. Men in South Africa, tend to be sicker than women when presenting for medical assistance including HIV counselling and testing services (HCT), because they access the services very late [7]. Fewer men test for HIV than women [8] and therefore risk transmitting HIV to other sexual partners unknowingly simply because they do not know their HIV status.
Men in South Africa, compared to their female counterparts, are more likely to die of AIDS-related causes, as well as tuberculosis [7], because fewer men are started and remain on HIV treatment. Therefore, HIV counselling and testing remains a very important access point for men into HIV treatment and care. Literature shows that HCT is a cornerstone to HIV prevention in general, and it has the potential of preventing HIV transmission [9]. According to another study [10] if HCT service is utilised, it will serve as a gateway to comprehensive HIV care and support including access to antiretroviral therapy (ART). HCT is therefore vital, as it offers males the benefit of knowing their HIV status and further assists them to plan for a longer, healthier life by making changes to their diets and lifestyle, should they test positive to HIV.
Factors, which contributed to low uptake of HCT amongst men includes proximity to a clinic, the belief that knowledge of an HIV infection may accelerate the disease progression, psychosocial factors such as HIV-related stigma and discrimination as well as confidentiality concerns [11]. HIV- related stigma and discrimination that is related to the healthcare facility and being attended to by a female healthcare workers, are some of the factors that prevent men from accessing HIV services, including HCT [12]. Social and community norms such as beliefs on what defines ‘manhood’, culture, perceptions of treatments, and other belief systems have also been found to influence men’s behaviour when it comes to seeking medical help [13]. Education about HIV and access to HCT needs to be improved amongst men in order to increase the the uptake of HCT as an important step for initiation of treatment [14].Low utilisation of HCT services will impact negatively on the health of individuals and the community, which could potentially lead to new HIV infections. This article therefore hopes to bring new insights into ways on how we could involve men in HIV prevention, treatment and care programmes.
2. METHODOLOGY
2.1. Study Design
A cross-sectional descriptive quantitative study; a survey where the representative sample of the population was studied at a single point in time.
2.2. Population and Sampling
The target population consisted of males (15 to 49 years old), who utilised and attended health services at health facilities, and who are sexually active group of people in Rustenburg Sub-district. A convenience sampling technique was used to select the sample. A Raosoft calculator was used to determine the sample size, with a 5% margin of error and 95% confidence level, the sample size was 383, which was raised by 10% to cater for incomplete questionnaires. The total sample size was 422.
2.3. Data Collection Instrument
A standardised self-administered questionnaire was used in the collection of data. The tool was written in English and translated to Setswana (the local language); the research team were responsible for data collection. The tool was divided into three parts: the first part consisted of demographic background of the participants, the second part deals with factors affecting HCT uptake while the third part covers pre-existing knowledge of the participants relating to HCT services.
2.4. Data Collection
The study participants were recruited from health facilities in Rustenburg cluster after ethical clearance had been obtained from Sefako Makgatho Health Sciences University and the Facility Managers of the health facilities. The research team visited the health facility and gave a presentation about the purpose of the study, the selection criteria, and data collection. Those who agreed (verbally) to participate were given consent forms to sign. and only those who signed the informed consent participated in the study. Recruitment of participants continued until the sample size was reached. The research team was available to assist during the filling-up of the questionnaires.
2.5. Validity and Reliability
A standardised tool was used as adapted from a previous study [14]. The research team pre-tested the tool at health facilities in Rustenburg sub-district, to rule out ambiguous questions. Approximately 10-15 participants in the study population participated in pre-testing of the tool. To increase reliability, the participants completed the questionnaire anonymously. The method used to collect data was the same across participants. Response bias could be introduced if the questions favoured one response over the other or if participants believed certain responses were desirable to the research team, and it was mitigated by ensuring anonymity of the responses and participants were able to answer questions freely.
2.6. Data Analysis
Data was extracted and captured into a Microsoft Excel spreadsheet. The data were validated by referring to the hard copies of the data collection sheets. The data was then imported into small STATA version 13. All digital information was kept on a password protected computer. All hard copies of the consent forms and questionnaires were kept in a cupboard and secured with a lock. All questionnaires were anonymised, with no names or other identifiers. All categorical variables such as gender and level of acceptability were analysed using frequency tables. For computing, the chi-square test was used to measure the level of significance at P<0.05. After conducting the chi-square test, the relevant statistically significant variables were included in a logistic regression model for further analysis.
2.7. Ethical Considerations
Ethical clearance was obtained from Sefako Makgatho Health Sciences University Research and Ethics Committee (SMUREC) reference number SMUREC/H/17/2018: PG. Permission to conduct the study was sought from the North-West Department of Health after ethical clearance was obtained. Additionally, permission was requested from the Facility Manager. All participants signed informant consent and confidentiality was maintained.
The study involved only those participants who met the selection criteria. The participants were given information about the study, they first agreed to participate voluntarily. Those agreed were then provided with an informed consent form to sign, and the questionnaires were kept anonymous by using codes as an identification of the respondents instead of real names. The participants were further given respect and privacy to promote free completion of questionnaire. The participants were reassured of their anonymous status, before and after the completion of the questionnaire. They were allowed and given an option to withdraw from the study at any time they wished to do so.
3. RESULTS
3.1. Sample Characteristics
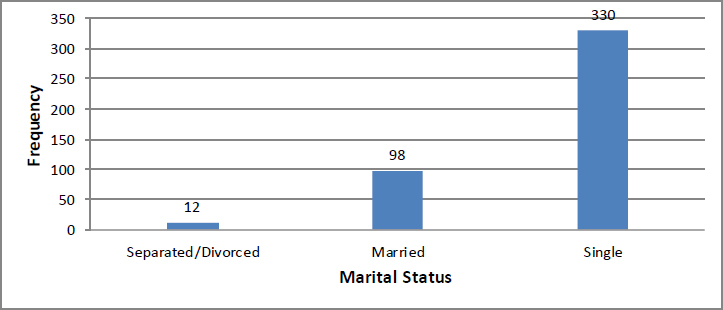
Four hundred and fifty (450) questionnaires were distributed to the participants aged between 15 and 49 years who visited selected health care facilities. Four hundred and forty (440) questionnaires were completed and returned giving a response rate of 98%. The average age was 33 years with a standard deviation of nine (9) years. The minimum and maximum age of participants was 15 years and 49 years respectively. The majority (n=162; 36.8%) of the study participants were aged between 30 and 39 years followed by those aged between 15 and 29 years (n=156; 35.5%) and those aged between 40 and 49 years (n=122; 27.7%). More than half of the sampled population were unemployed (n=230; 52.3%) and the remainder (n=210; 47.7%) were employed. Most of the participants said that they lived with their partners (n=137; 31.1%). Ninety-eight (22.3%) lived with parents, 91 (20.7%) lived with others and 56 (12.7%) lived with siblings; while forty-eight (10.9%) indicated that they were staying with their mothers, and only 10 (2.3%) resided with their fathers. The findings indicated that most of the participants (n=330; 75%) were single, ninety-eight (22.3%) were married, and 12 (2.7%) were divorced or separated from their partners (as reflected in Fig. 1).
| Questionnaire Item | Agreen (%) | Disagreen (%) | Don’t known (%) |
|---|---|---|---|
| Location influences testing | 318 (72.3) | 52 (11.8) | 70 (15.9) |
| HCT important in the fight against HIV/AIDS | 386 (87.7) | 22 (5.0) | 32 (7.3) |
| Adequate information about test | 322 (73.2) | 69 (15.7) | 49 (11.1) |
| Know where to find free test | 385 (87.5) | 32 (7.3) | 23 (5.2) |
| Comfortable using HCT services in future | 365 (83.0) | 35 (8.0) | 40 (9.0) |
| Heard about HCT | 328 (74.5) | 112 (25.5) | 0.0 (0) |
| Willing to take up HCT | 384 (87.2) | 31 (7.1) | 25 (5.7) |
| Pre-test counselling necessary | 357 (81.1) | 46 (10.4) | 37 (8.4) |
| Post-test counselling necessary | 314 (71.4) | 63 (14.3) | 63 (14.3) |
| Information leaflet sufficient for HCT | 295 (67.0) | 33 (7.5) | 112 (25.5) |
| Were you aware of provision of HCT in facility | 298 (67.7) | 105 (23.9) | 37 (8.4) |
| Was HCT offered during your visit in facility | 300 (68.2) | 97 (22.0) | 43 (9.8) |
| Was the language used in facility understood | 405 (92.0) | 21 (4.8) | 14 (3.2) |
3.2. Uptake of HCT Services
Our findings indicate that most of the participants (n=401; 91.14%) had been tested for HIV. The trends in the usage of HCT services were further clarified by breaking down the totals into respective sub-totals following cross-analysis using their demographic characteristics and other relevant variables.
3.3. Knowledge and Opinion on HCT Services
Most of the participants (n=264; 65.8%) preferred to be tested for HIV at a clinic and only 55 (13.7%) were tested during an HIV testing campaign. The reasons for testing varied, with the highest proportion (n=317; 79.1%) saying that they were tested to know their HIV status. The number of those tested because they were sexually active were (n=31; 7.7%) while those who tested together with their partners were (n=33; 8.2%). Most of participants (n=350; 87.3%) who took part in the study agreed that they were satisfied with the quality of service they received. Nineteen (4.7%) said that they were not satisfied whilst 32 (8.0%) said they were somewhat satisfied. Health facilities appear to be the most widely used establishments for accessing health-related services for the communities in this study. Three hundred and eighty-four (87.3%) of participants indicated that they use public health facilities whilst 39 (8.9%) participants indicated that they use private healthcare establishments and 17 (3.8%) accessed health services during campaigns.
Majority of the participants (n=386; 87.7%) agreed that HIV testing is important in the fight against the disease, whilst 22 (5.0%) disagreed, and 32 (7.3%) had no knowledge regarding HIV. Most of the participants (n=328; 74.5%) indicated that they had heard about HCT whilst 112 (25.5%) reported that they were yet to hear about HCT. On the different factors that affect the uptake of HCT services, most of the participants (n=318; 72.3%) agreed that the location of the test centre had impacts on HIV testing tendencies. Most of the participants (n=365; 83.0%) indicated that they would be comfortable with using HCT services in future. Most of the participants (n=298; 67.7%) were aware that HCT services were offered at health care facilities within their communities. Most of the participants (n=385; 87.5%) knew where to access free HIV testing services; while a smaller number (n=23; 5.2%) were not aware of where free HCT can be accessed (Table 1).
3.3.1. Relationship between Knowledge on HCT Services and Participant’s Demographic Characteristics
Findings on the relationship between knowledge about HCT, as indicated by responses to the question “Have you heard about HCT services”, and demographic variables: age category, employment status, living arrangement, marital status, and level of education. Pearson’s Chi-square test was performed on the responses of all the study participants (n=440), (Table 2).
| Variable | - | NoN (%) | YesN (%) | d.f | X2 | P-value |
|---|---|---|---|---|---|---|
| a). Age category | 15-29 years | 59 (37.82) | 97 (62.18) | 2 | 20.0573 | 0.000* |
| 30-39 years | 33 (20.37) | 129 (79.63) | - | - | - | |
| 40-49 years | 20 (16.39) | 102 (83.61) | - | - | - | |
| b). Employment status | Employed | 39 (18.57) | 171 (81.43) | 1 | 10.0306 | 0.002* |
| Unemployed | 73 (31.74) | 157 (68.26) | - | - | - | |
| c). Living arrangement | Parents | 33 (33.67) | 65 (66.33) | 5 | 9.3861 | 0.095 |
| Mother | 15 (31.25) | 33 (68.75) | - | - | - | |
| Father | 2 (20.00) | 8 (80.00) | - | - | - | |
| Partner | 24 (17.52) | 113 (82.48) | - | - | - | |
| Sibling | 13 (23.21) | 43 (76.79) | - | - | - | |
| Other | 25 (27.47) | 66 (72.53) | - | - | - | |
| d). Marital status | Married | 18 (18.37) | 80 (81.63) | 2 | 3.5616 | 0 .169 |
| Single | 90 (27.27) | 240 (72.73) | - | - | - | |
| Divorced orSeparated | 4 (33.33) | 8 (66.67) | - | - | - | |
| e). Level of education | No school | 5 (26.32) | 14 (73.68) | 5 | 9.2315 | 0 .100 |
| Primary | 7 (27.17) | 17 (70.83) | - | - | - | |
| Secondary | 50 (31.06) | 111 (68.94) | - | - | - | |
| Grade 12 | 44 (24.31) | 137 (75.69) | - | - | - | |
| Tertiary | 6 (11.32) | 47 (88.68) | - | - | - | |
| Don’t know | 0 (0) | 2 (100) | - | - | - |
| DemographicVariable | Category | Knowing Statusn (%) | Freely Accessiblen (%) | Incentiven (%) | Totaln(%) | d.f | X2 | P-value |
|---|---|---|---|---|---|---|---|---|
| a. Age | 15-29 years | 128(82.05) | 15(9.62) | 13(8.33) | 440 | 4 | 10.80 | 0.029* |
| 30-39 years | 140(86.42) | 16(9.88) | 6(3.70) | |||||
| 40-49 years | 113(92.62) | 8(6.56) | 1(0.82) | |||||
| b. Employment Status | Employed | 186(88.57) | 17(8.10) | 7(3.33) | 440 | 2 | 1.75 | 0.417 |
| Unemployed | 195(84.78) | 22(9.57) | 13(5.65) | |||||
| c. Living arrangement | Parents | 73(74.49) | 15(15.31) | 10(10.20) | 440 | 10 | 19.25 | 0.037* |
| Mother | 42(87.50) | 4(8.33) | 2(4.17) | |||||
| Father | 10(100.00) | 0(0.00) | 0(0.00) | |||||
| Partner | 121(88.32) | 12(8.76) | 4(2.92) | |||||
| Sibling | 52(92.86) | 3(5.36) | 1(1.79) | |||||
| Other | 83(91.21) | 5(5.49) | 3(3.30) | |||||
| d. Marital status | Married | 83(84.69) | 12(12.24) | 3(3.06) | 440 | 4 | 3.50 | 0.477 |
| Single | 287(86.97) | 27(8.18) | 16(4.85) | |||||
| Divorced or Separated | 11(91.67) | 0(0.00) | 1(8.33) | |||||
| e. Level of education | No school | 18(94.74) | 0 (0.00) | 1(5.26) | 440 | 10 | 9.28 | 0.506 |
| Primary | 20(83.33) | 1(4.17) | 3(12.50) | |||||
| Secondary | 136(84.47) | 17(10.56) | 8(4.97) | |||||
| Grade 12 | 160(88.40) | 14(7.73) | 7(3.87) | |||||
| Tertiary | 45(84.91) | 7(13.21) | 1(1.89) | |||||
| Don’t know | 2(100.00) | 0(0.00) | 0(0.00) |
| Variable | Comparison between | and | OR | P-value | 95% C.I |
|---|---|---|---|---|---|
| a. Ease of testing | Not easy | Very easy | 2.250 | 0.029 | 1.085 – 4.665 |
| Somewhat easy | 1.058 | 0.907 | 0.4095 – 2.734 | ||
| b. Information about test | No | Yes | 3.702 | 0.001 | 1.730 – 7.923 |
| Unsure | 1.393 | 0.517 | 0.511 – 3.794 | ||
| c. Know where to find free test | No | Yes | 3.437 | 0.009 | 1.370 – 8.622 |
| Unsure | 1.867 | 0.407 | 0.4271 – 8.158 | ||
| d. Heard about HCT services | No | Yes | 5.039 | 0.000 | 2.553 – 9.948 |
4. DISCUSSION
This study examined factors that are associated with poor uptake of HIV counselling and HIV testing among participants that used health facilities in Rustenburg sub district.
4.1. HCT in Relation to Participants’ Age
Awareness of HIV sero-status is viewed as an important element of HIV treatment and prevention efforts. A study [15, 16] noted that achieving a universal HIV-status awareness is a critical step in ensuring that HIV-infected individuals are afforded access to antiretroviral treatment (ART) to achieve effective virological suppression and delayed diagnosing is posing challenges to the health of HIV positive individual [17].
The results of our study indicated that men aged between 40 and 49 years were more likely to get tested for HIV than other age groups. Early testing in South African communities is very important given that the boys in their early stage start having sex. For instance, it was reported that men aged between 15 and 24 years in KwaZulu Natal had their first sexual encounter before 15 years while others as early as 9 years of age. These encounters constitute high risk for HIV infection, especially that most of the participants did not know their first sexual partners [18]. Lower testing rates in adults aged 15 to 29 is disturbing since young people have a high risk-seeking propensity [19]. Youth and young adults were more likely to engage in activities that put them at risk of contracting HIV infection (activities such as binge alcohol drinking, experimentation with drugs and having unprotected sex) [20]. It is our opinion that getting young men to test for HIV would undoubtedly increase the success of HIV prevention.
4.2. HCT in Relation to Participant’s Employment Status and Education
It was observed that employed people were more likely to get tested for HIV. There was no direct link between being employed and the likelihood of getting tested. It was observed that those who were employed were more likely to be educated than unemployed [21]. It has been shown that individuals who are more educated are more likely to get tested [22]. In the current study, the findings agreed with results of other study [21]. Those with tertiary educations were the most likely to be tested followed by those with secondary education. Participants with higher level of education are more likely to distinguish between facts and myths with respect to HIV. In certain sub-Sahara countries, such as Ghana [23], South Africa [24], and Malawi [25], studies show that facts about HIV have been misinterpreted by respondents [26, 27].
4.3. HCT in Relation to Marital Status of Men
This study shows that married participants were more likely to get tested than single, divorced and separated participants. This agrees with the findings of other studies [28, 29] who reported that men in general do not like getting tested for HIV and that young single men were less likely to get tested. This observation is important because marriage has been reported as a risk factor in acquiring HIV infection since married couple seldom use condoms and infidelity in marriages is now common place [30]. The connection between HIV and marriage was even stronger in some African communities, where polygamy is still being practiced [31]. The observation that unmarried men were less likely to test is not good for HIV prevention efforts.
4.4. Reasons for Undertaking HIV Testing
Of the 440 participants who took part in the study, 8.9% (n=39) had not been tested for HIV and provided reasons for their action:
4.5. Fear of Knowing one’s HIV Status
A study [11] reported that men were afraid of getting tested for HIV, because they felt that being diagnosed with HIV would result in lifestyle changes, uncomfortable lifestyles, and identity changes. Our study revealed that the fear was the main reason (n=10; 25.6%) why participants in this study did not like getting tested. One major implication of this is that men are likely to start ART at later stages of the disease and are more likely to die earlier than women with the same condition. Another study [31] reported that the fear of getting tested stems from an ill-informed position which equate positive HIV diagnosis to a death sentence. A study conducted in Cote d’Ivoire [32] found that men were afraid of getting tested because being HIV positive made them feel less masculine. They further stated that the masculinity of men, hinges on five domains, social standing, family, sexuality, health and work, and their fear was that being HIV positive threatens all these domains. Due to distress and uncertainty that HIV creates in the lives of HIV positive, fear and anxiety are universal problem for these individuals [33, 34].
4.6. Stigmatisation
HIV/AIDS stigma is a serious matter because it affects the psychological well-being of HIV positive people making other treatments less effective [35]. Our study revealed that only 10.2% (n=4) of the study participants declined to be tested due to fear of being stigmatised if HIV positive. Musheke et al. [36] provided reasons behind poor uptake of HIV testing services in sub-Sahara Africa and noted that stigmatisation is one of the major hindrances to people being tested. It was important to note that sustained programmes by different institutions to eliminate stigmatisation could be paying off hence the observed outcome in our study. Studies from across the globe revealed three main causes of HIV-related stigma in health facilities; lack of awareness was one of the factors [37]. The argument that communities are aware of HIV/AIDS and related issues could further be supported by the observation that 87.7% (n=386) of the study participants had adequate information about HCT services. The South African government, together with other partners, have deployed resources in response to HIV crisis in order to increase awareness [26] to tackle stigmatization and it appears to be bearing positive results.
4.7. Service Delivery and Uptake of HCT Services
The avenue through which HCT services were delivered was an important factor in promoting engagement across HIV treatment continuum [38, 39]. In our study, most of the participants (n=264; 65.8%) tested for HIV at local clinics. services. In some countries such as Zimbabwe, there were centres specifically for HIV testing and a model preferred in areas where stigma was perceived to be high [40]. It has been noted that, often, young people were not willing to exploit available healthcare services including, HCT services, due to perceived or actual barriers of accessibility, concerns regarding confidentiality, overburdened healthcare systems, and stigma. It can be assumed that increasing stand-alone HCT centres will increase the number of young adults getting tested for HIV [41].
Our study found that those who felt that “it was easy to get tested” were more likely to be tested than those who felt otherwise and many of the participants were willing to be tested again. This had two implications. First, it can be taken as an endorsement of the services offered by the healthcare centres. Secondly, the participants were willing to be retested again in the future. Repeat testing for HIV has the potential of reducing the rate of spread of the infection and allows an individual to commence ART quicker. Late initiation of ART was significantly associated with a poor response to treatment, an increased risk of progression from HIV seropositive to full blown AIDS as well as mortality [42]. Another important factor related to uptake of HCT services is the distance a test site was in relation to the residential area of the clients. The results of our study showed that the participants’ tendency to get tested was dependent on the distance to respective test centres. This agreed with the findings of a study [43] who reported that people seeking to be tested for HIV tests chose service providers who were accessible at distance not far from their residents.
4.8. HCT Services in Relation to Participant’s Demographic Characteristics.
Odds ratios (OR) were calculated to assess differences, or similarities of the likelihood of getting tested for people in different demographic categories. Results showed that men aged between 30 and 39 years as well as those between 40 and 49 years were approximately twice as likely to get tested for HIV compared to those aged between 15 and 29 years [44]. This was consistent with the finding from another study [45].
5. LIMITATIONS OF THE STUDY
This is a cross-sectional study and only looked at the situation obtained at a single point in time. This limited the strength of inferences that could be made from the results. The responses received from participants were made from their own personal experiences and interactions with health facilities. Therefore, the participants’ knowledge and understanding of middleics around HIV is subjective and represent their opinions. The study focused on a specific subset of males aged between 15 and 49 years based in Rustenburg and those who visited the health facilities. It does not represent the full population of adult males in Rustenburg. The study employed convenience sampling method which may not fully represent the male population in Rustenburg. Despite the limitations described, this study provided an understanding and insight into the factors associated with poor uptake of HCT services among males in health facilities in Rustenburg sub district.
CONCLUSION
The findings of this study suggest that various factors are associated with HCT uptake such as age, knowledge about the availability of HCT services, employment status and who a participant was living with. The result showed that age is significantly associated with knowledge, motivation for HIV testing and usage of HCT services.
RECOMMENDATION
A direct link between masculinity, fear of stigma and traditional beliefs and uptake could not be established in this study. A further qualitative study would be necessary to assess the attitudes, values and beliefs held by adult males which could potentially affect their HCT uptake. The study could also not determine what the participants’ thoughts were about confidentiality. Therefore, a further qualitative study would also be necessary to assess the beliefs related to confidentiality. Research on HIV self-testing and its effect on uptake of HCT amongst men will need to be undertaken to fully understand the link between the two. Whilst the feelings of the participants around testing were studied, their experiences and interaction with health facilities were not studied. Further research into this and its impact on uptake will need to be done to assess this. In our study, it is not clear when participants first got tested. It will be more informative if an another study looks at the rate or frequency of repeat testing in the community. It will also provide a better measure on the uptake of HIV testing services. African culture is characterised by traditional beliefs that have been observed to hinder the uptake of HIV testing services. There is a need for a study that looks at these beliefs and how they could be managed such that the 90-90-90 targets would be met.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Ethical clearance was obtained from Sefako Makgatho Health Sciences University Research and Ethics Committee (SMUREC) reference number SMUREC/H/17/2018: PG. Permission to conduct the study was sought from the North-West Department of Health after ethical clearance was obtained. Additionally, permission was requested from the Facility Manager. All participants signed informant consent and confidentiality was maintained.
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committee and with the 1975 Declaration of Helsinki, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from all participants.
STANDARDS OF REPORTING
STROBE guidelines were followed.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information is available within the article.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


