All published articles of this journal are available on ScienceDirect.
Cutaneous Anthrax in a Farmer Man: A Case Report
Abstract
Introduction:
Anthrax is an acute infection caused by Bacillus anthracis, an anaerobic, spore-forming, Gram-positive bacterium. Anthrax disease is a common disease among herbivores and humans that is transmitted to humans through direct contact with farm animals that are sick or have died of anthrax.
Case Summary:
A 43-year-old man having livestock as a profession had a cutaneous anthrax infection on the dorsal surface of his left thumb. The patient was infected with anthrax by slaughtering a sheep infected with Bacillus anthracis. He was treated with penicillin after an early diagnosis of anthrax bacillus.
Conclusion:
Anthrax infection is a highly contagious disease, and early detection is very important. There is a need to strengthen the health care system for farm animals and educate farmers on how not to consume the meat of diseased carcasses and how to dispose them of hygienically, especially in high-risk areas.
1. INTRODUCTION
Anthrax is an infectious disease; 2,000 cutaneous anthrax cases are reported worldwide each year [1]. It is an animal disease; human anthrax is rare, and it is rarely the cause of serious human disease. The spores of the bacterium B. anthracis enter the body through damaged skin or through inhalation and digestion [2, 3]. On the other hand, anthrax is an occupational disease and is transmitted in both industrial and agricultural forms [4]. The agricultural form is common among ranchers, butchers, and veterinarians who work with farm animals, and its industrial form is common among those working in the tannery, wool spinning, and animal product processing industries; all of these industries carry pollution from the livestock source [5]. Most human anthrax cases are occupational; for example, people who raise wild animals are at risk; humans become infected through contact with animals or through contact with their products such as wool [6]. After contact with nutrient media such as animal or human tissues or blood, the spores become vegetative and become active bacilli [7]. On the other hand, bacilli never become spores in the body of living hosts; however, the formation of spores is impaired. This becomes possible when contaminated secretions and tissues are exposed to air [7]. The cutaneous form of anthrax begins with itchy papules and develops into a wound surrounded by vesicles and pustules within 12 days, and then a black necrotic scar develops [8]. The lesions are usually painless, and there may be lymphadenopathy in the area [8]. Diagnosis of the disease is based on the contact with the source of infection and the patient's occupation, the shape and course of skin lesions, and smear, and culture of wound secretions.
2. CASE PRESENTATION
2.1. Patient Information
A 43-year-old man with a livestock occupation had a cutaneous anthrax infection that affected the dorsal surface of the left thumb. The patient was infected with anthrax by slaughtering a sheep infected with Bacillus anthracis.
2.2. Clinical Findings
A vesicular lesion and blister were formed on the dorsal surface of the index finger of this patient's left thumb without any pain, but there was itching; the patient showed no fever, lethargy, adenopathy, or lymphangitis and showed no pain on palpation upon examination and diagnosis.
2.3. Diagnostic Assessment
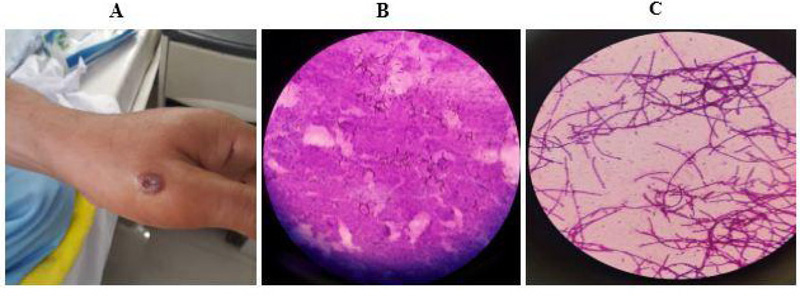
Microbiological tests with swabs and culture were performed on the patient with suspected cutaneous anthrax. Gram staining of the wound confirmed the diagnosis. During this staining, spore-forming gram-positive bacilli were reported that matched B. anthracis (Fig. 1). For the patient, an intravenous crystal antibiotic drug was started at a dose of two million units every 6 hours.
3. DISCUSSION
Despite anthrax control in developed countries, the disease remains a health problem in developing countries [9]. According to previous study reports, more than 95% of anthrax infections worldwide are cutaneous anthrax [2, 10, 11]. More than 90% of injuries occur in exposed areas such as the face, neck, arms, and hands. Anthrax is named after the characteristic black scars it leaves behind [12]. Anthrax is an anthropozoonotic disease that is rare in developed countries. Most of the patients with this disease had a history of contact with animals and animal products [13]. Initially, the skin lesions are pink papules that appear 3 to 5 days after contact; then, within 36 hours, the lesion is marked as a vesicle with central necrosis, typical black scars, and peripheral edema; it can be associated with lymphadenopathy and leave a permanent scar even after recovery [14]. Serological tests are positive 10 days after the onset of symptoms, and their maximum titer is 40 days [15]. Mortality from cutaneous anthrax is up to 20% without antibiotic treatment but is reduced to zero with appropriate antimicrobial treatment [16, 17]. Although antibiotic treatment does not change the course of the skin lesion, it does reduce the risk of systemic disease. More recently, in the United States, due to the simultaneous cutaneous and respiratory anthrax hypothesis and the long latency of the disease, antibiotic therapy has been prescribed for at least 60 days instead of 7-10 days. Ciprofloxacin 500 mg twice daily, doxycycline 100 mg twice daily, or amoxicillin 500 mg three times daily are recommended [18]. Penicillin has been our drug of choice in studies over time, and resistance to penicillin has proven to be very rare [18]. After treating cutaneous anthrax, sterile lesions, and scar tissue for 24 hours, chloramphenicol, erythromycin, tetracycline, or ciprofloxacin may be prescribed for penicillin allergy sufferers. For patients who are resistant to penicillin and doxycycline, ciprofloxacin is another option. 10 days after the appearance of the lesions in the treated patients, the lesion slowly begins to disappear, with a maximum duration of 26 weeks [18]. In the disposal of anthrax (animal) carcasses in most countries, the preferred method of disposal is incineration. Controlled heat treatment or “rendering” has been proposed in at least one country of the European Union, but no records of it being done or of relevant legislative documentation have been identified. Where neither of these approaches is possible, for example, owing to lack of fuel, burial is the remaining less satisfactory alternative [19].
CONCLUSION
Anthrax is a serious zoonotic disease that can affect most mammals and several species of birds but is particularly observed in herbivores. Anthrax infection is a highly contagious disease, and early detection is very important. There is a need to strengthen the health care system for farm animals and educate farmers on how not to consume the meat of diseased carcasses and how to dispose them of hygienically, especially in high-risk areas.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
All procedures were approved by Ayatollah Alimoradiyan Hospital, Nahavand, Hamadan, Iran (P.16.41.13.1354).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
Informed consent was obtained from the participant.
AVAILABILITY OF DATA AND MATERIALS
Not applicable.
STANDARDS OF REPORTING
CARE guidelines have been followed.
FUNDING
None.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The author would like to thank all members of laboratory medicine of Ayatollah Alimoradiyan Hospital, Nahavand, Hamadan, Iran.


