All published articles of this journal are available on ScienceDirect.
Actinotignum schaalii and Aerococcus urinae as Etiology of Infected Kidney Cyst: A Diagnostic Challenge
Abstract
The case presented here illustrates a sometimes complex disease presentation where interdisciplinary teamwork is essential. A 74-years-old woman with stable chronic obstructive pulmonary lung disease and a composite graft aortic valve implant was admitted to hospital with an episode of acute lower back pain combined with long-term fever. The final diagnoses of a left-sided, infected and radiologically evident kidney cyst caused by the urinary tract pathogens Actinotignum schaalii and Aerococcus urinae was established by the use of partial 16S/18S rRNA gene sequence analysis on kidney cyst drainage material taken after four weeks of relevant antibiotic therapy.
1. INTRODUCTION
Recognition and identification of the causative agents have long been a cornerstone in the management of serious infections. For many years this has primarily relied on traditional culturing methods. Within the last two decades, the microbiological diagnostic repertoire has expanded dramatically especially due to the rapid development of molecular tests based on genomics and proteomics. Detection of DNA directly from different types of human specimens based on the use of partial 16S/18S rRNA gene sequence analysis has made it possible to detect an infectious etiology even when antibiotic treatment has been instituted [1]. Comparing proteomic content of strains of bacteria and fungi using Matrix-assisted Laser Desorption/Ionization-TOF (MALDI-TOF) mass spectrometry has improved accurate and quick species identification [2]. Therefore, recognition of difficult to detect infections and identification of rare and difficult to identify microorganisms have improved substantially.
The two species Aerococcus urinae and Actinotignum schaalii have especially been associated with infections related to the urinary tract. They are both described as fastidious organisms that may need special care for growth and, therefore, detection [3-7].
Here, we report a challenging case of a kidney cyst infected by both bacteria and discuss it in a multidisciplinary perspective. Both molecular methods mentioned above were used to establish the diagnosis.
2. CASE REPORT
A 74-years-old woman, with chronic obstructive pulmonary lung disease, osteoporosis, hypercholesterolemia and hypertension, who had undergone trans-catheter aortic valve implantation 5 months ago, was admitted to the local hospital in the Zealand region, Denmark. She presented severe pain in the lower part of the back for less than 24 hours without radiation to the lower limbs. The severity of the pain was noted as 9 on a 10-point Visual Analogue Scale. Prior to admission, she had a low grade fever (37 - 38ºC) for about four weeks.
On admission, the patient was febrile (38.8˚C) and had lumbar paints at L3 level on examination, but without specific findings otherwise. By palpation, bilateral lumbar muscular tenderness was noticed. There was no tenderness of spinous process, but pronounced painfulness related to the left lower back. A blood pressure of 157/86 mm Hg and a heart rate of 92 per minute was noticed. The blood-leucocyte count on admission was 13.6 x 109/L (reference interval 3.5 – 8.8 x 109/L) of which 11.1 x 109/L were polymorphonuclear neutrophils, with a C-reactive protein (CRP) reaction of 152 mg/L (reference interval < 8 mg/L). A urine point-of-care test showed no signs of infection.
At admission, no specific explanation for the lumbar pains was recognized though the patient was febrile and had elevated infection parameters. Based on the above, no definitive diagnosis could be established. The differential diagnoses included: 1) infective spondylodiscitis, 2) infective endocarditis, 3) lung infection and 4) colonic diverticulitis. Later on, vaginal cancer was considered after the discovery of a vaginal cyst measured 3.3 x 2.2 x 2.0 cm by ultrasonography and elevated cancer antigen (CA)-125 of 47 kU/L (reference interval <35 kU/L).
Blood cultures (1 bottle out of 3) taken on admission were positive after 2 days of incubation with the growth of Gram-positive cocci in clusters, later described as A. urinae. Initial microscopy of the positive blood culture gave a suspicion of staphylococci, which supporting the suspicion of spondylodiscitis. Unfortunately, no urine culture was taken initially. Chest and lumbar X-rays as well as MR-scan of the spine performed two days after admission, only revealed a previously known reduced height of corpus of TH12 but showed no signs of infection.
The growth of A. urinae in the blood supported suspicion of urinary tract infection (UTI) and infective endocarditis; however urine culture taken on the fourth day was without growth. A transesophagal echocardiography done one day after the definitive identification of A. urinae was without signs of infective endocarditis. A PET/CT (Positron emission tomography–computed tomography) scan performed on day 15 revealed a metabolic active focus with callous periphery in the left upper part of the left kidney that measured 5 x 6,7 x 5,6 cm (horseshoe appearance) and was suspected of being an infected cyst/abscess. No signs of hydronephrosis were found. Additional findings were infiltrates of left upper and right lower pulmonary lobes (probably infectious), a suspicion of Bartholinitis and colonic diverticulitis, hypermetabolism in the periphery, the aortic valve graft and presence of small, but metabolic active, thoracic and retroperitoneal lymphnodes. In conclusion, a focus related to the kidneys was suspected.
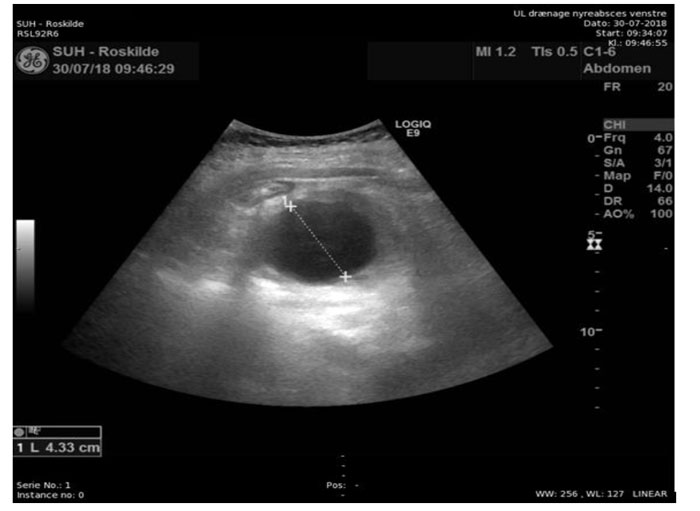
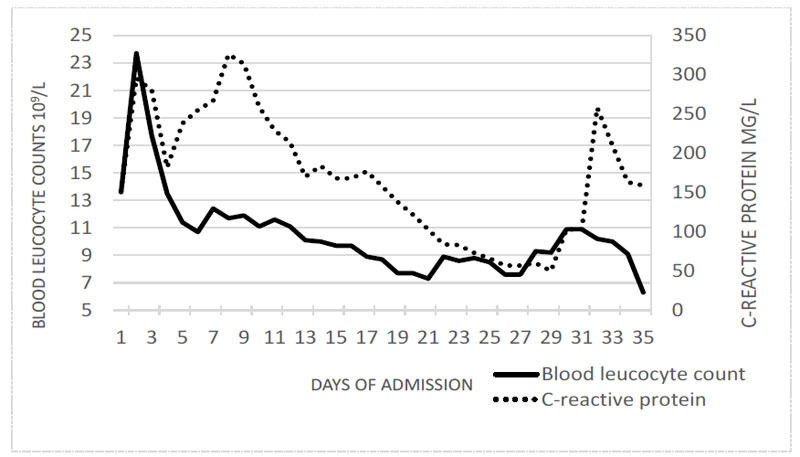
Empirical antibiotic treatment included initial intravenous (iv.) piperacillin/tazobactam (4g TID) and iv. cefuroxime (3 g TID) given shortly on suspicion of infective endocarditis caused by staphylococci. Further treatment included iv. penicillin (5 mill.IE QID) and gentamycin (3 mg/kg QD) until infective endocarditis was excluded followed by iv. penicillin (3 mill. IE TID) for four weeks. Nevertheless, the patient remained intermittently febrile with elevated though declining CRP. Four weeks after admission (on the 29th day of admission) ultrasound guided drainage of the abscess (50 ml) was performed (Fig. 1). The drain was left in place for four days and used for rinsing the abscess five times daily. Bacterial culture of the abscess content remained without growth, but molecular examination demonstrated DNA from A. urinae as well as A. schaalii (see the section Microbiology). Blood-leucocyte counts and CRP reactions fluctuated during the 6 weeks of hospitalization though gradually declining. At discharge a blood-leucocyte count of 6.3 x 109/L and a CRP reaction of 159 mg/L was noticed (Fig. 2) leading to further 10 days of treatment with oral phenoxymethyl-penicillin (1 mill. IE QID) and piv-mecillinam (400 mg TID). The latter due to the growth of Eschericia coli in a urine culture drawn from catheter-a-demeure. After discharge, two episodes with suspicion of infected cyst have occurred with the immediate effect of antibiotic therapy.
3. MICROBIOLOGY
3.1. Culture Examinations
Blood culture examinations: On the second day of incubation, 1 of 6 blood culture bottles (BACT/ALERT® FAN Aerobic - Biomérieux) taken at admission became positive. Microscopy revealed Gram-positive cocci in clusters resembling staphylococci. When grown in ambient air supplemented with 5% CO2 on chocolate agar, and on Danish Horse-blood Agar, the culture showed after one day pin-point alpha-hemolytic colonies increasing to 2 mm after 2 days incubation.
Mass spectrometry (Bruker Daltonics using MBT Compass software version 4.1 that contains 6903 MSP´s) identified the strain as A. urinae with a score of 2.12 (with 10 identical next hits). Antimicrobial susceptibility testing was done using agar diffusion disc methodology (Oxoid, UK), as described and recommended by the European Committee on Antimicrobial Susceptibility Testing for A. sanguinicola and A. urinae (penicillin, meropenem, ciprofloxacin and nitrofurantoin) and viridans group streptococci (piperacillin-tazobactam, cefuroxime, clindamycin) (www.eucast.org). The A. urinae strain was found sensitive to penicillin, piperacillin-tazobactam, cefuroxime, meropenem, ciprofloxacin, clindamycin and nitrofurantoin. Zone diameters to sulfonamides and trimethoprim were for both zero and the strain interpreted as being resistant. MICs (Etest, bioMérieux, France) of penicillin and gentamicin were 0.016 µg/ml and 4 µg/ml, respectively.
Six additional blood-culture sets (18 bottles in total) taken during hospitalization were without growth.
Other specimens being cultured: 1) Urine specimens at admission and additionally three while hospitalized were without growth while one specimen close to dismission gave growth of E. coli resistant to ampicillin but otherwise sensitive to beta-lactams, gentamicin and ciprofloxacin. 2) The below described kidney cyst drainage specimen was without bacterial growth prior to partial 16S/18S rRNA gene sequence analysis.
Partial 16S/18S rRNA gene sequence analysis of kidney cyst drainage specimen: The sample was processed using Micro-Dx™ kit in combination with SelectNA™ or SelectNA™ plus (Molzym GmbH & Co. KG, Bremen, Germany). The Micro-Dx™ kit contains primers targeting conserved regions of the 16S (V3 and V4 regions) and the 18S (regions V8 and V9) rRNA genes. Real-time PCR was run for 40 cycles. In short, tissue samples were pre-treated with proteinase K for 10 min. Body fluids, swabs and tissues were treated with a chaotropic buffer, lysing the human cells, and subjected to DNase treatment to degrade the human DNA. DNA from potentially present microorganisms was subsequently extracted in SelectNA™ or the SelectNA™ plus instrument and PCR-positive samples were sent to Eurofins GATC Biotech NPL (Cologne, Germany) for sequencing. Three sequencing primers were used: one optimized for gram positive, one optimized for gram negative bacteria, and the third for fungi. This assay makes it possible to identify up to two different bacteria and one fungus in one analysis. Returned sequencing data were edited and compared with deposited sequences in the NCBI database using the BLAST search engine. Both A. schaalii and A. urinae were identified. The number of identical bases, MaxScores and E-values were 413/413 (100%), 746 bits, 0.0 for the A. schaalii identification and 420/423 (99%), 738 bits, 0.0 for the A. urinae identification. For A. schaalii and A. urinae, respectively, the difference in max scores from best taxon match to next best taxon match, the number of identical best taxon matches and next best taxon matches were 29 and 36, 13 and 24, Actinobaculum sanguinis and Aerococcus christensenii.
4. DISCUSSION
The case presented here demonstrates the importance of interdisciplinary teamwork when dealing with complex, possibly multimorbid patients. Probable pulmonary, cardiac, gastro-intestinal, as well as urogenital involvements had to be cleared up. The growth of A. urinae in one of six blood-culture bottles taken on admission gave a suspicion of a urogenital focus. A. urinae is a known cause of infective endocarditis [3] and involvement of the aortic valve graft had to be ruled out by echocardiography. Though previously described, a marked reduced height of corpus of TH12 could have had a relation to the observed back pain. The callous appearance of the periphery of the cyst may have influenced and hampered antibiotic distribution into the cyst. This might explain the slow response to the treatment, which lasted until external drainage of the cyst.
To the best of our knowledge, this is the first case report of an infected kidney cyst with either of the detected bacteria, both known uropathogens. A. urinae is a Gram-positive coccus resembling staphylococci by microscopy and fastidious alpha-hemolytic streptococci by growth [4]. It has primarily been implicated in less than 1% of all symptomatic urinary tract infections, especially in elderly men [7], causing severe and invasive infections including urosepticemia and infective endocarditis [3, 4]. Sporadic cases of soft tissue infections mostly, but not exclusively, with relation to the urinary tract have been reported [8, 9]. Both species mentioned are thought to be part of the urogenital microbiota. A. schaalii (formerly Actinobaculum) is a small, Gram-positive fastidious bacillus [5, 6, 10]. Its disease spectrum is much like the one described for A. urinae though the reported frequency has been much lower. Only one case of infective endocarditis with A. schaalii has been published. It is mostly been responsible for UTIs in young or elderly patients, particularly in patients with urological diseases.
CONCLUSION
This report illustrates a complex disease presentation where interdisciplinary teamwork is essential. The improving microbiological diagnostic repertoire especially within the fields of genomics and proteomics, has substantially upgraded diagnostic possibilities. In our case, molecular examination of drainage material from a kidney cyst obtained after four weeks of relevant antibiotic treatment was able to reveal the presence of DNA from the urinary tract pathogens A. schaalii and A. urinae.
ETHICAL APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Written informed consent was obtained from the patient.
STANDARD OF REPORTING
CARE guidelines and methodology were followed.
FUNDING
None
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


