All published articles of this journal are available on ScienceDirect.
Bacterial Culture Results and Antibiograms in Chronic Rhinosinusitis Patients in Mekong Delta, Vietnam
Abstract
Background
The inappropriate use of antibiotics for chronic rhinosinusitis, exceeding established guidelines, is a growing concern in Vietnam. This practice is contributing to the emergence and spread of antibiotic-resistant bacteria.
Objective
This study aimed to evaluate the results of culture and antibiogram of bacteria on patients in the Mekong Delta, Vietnam, who were treated for chronic rhinosinusitis in 2022-2023.
Methods
It is a cross-sectional study, including 113 patients who came for treatment with a diagnosis of chronic rhinosinusitis at Can Tho University of Medicine and Pharmacy Hospital, Mekong Delta, Vietnam, from 2022-2023. The bacterial cultures were identified, and their antibiograms were performed in the Microbiology laboratory of Can Tho University of Medicine and Pharmacy. Statistical analysis was performed with SPSS version 20.0.
Results
The rate of bacterial growth was 97.35%. The cultured bacterial composition had 8 genera, 22 species, and 116 samples, of which 2 bacterial species were cultured, accounting for 5.45%. Antibiogram showed that Streptococcus pneumonia was resistant to cefaclor (83.33%), cefuroxime (100%), trimethoprim+ sulfamethoxazole (100%), and susceptible to chloramphenicol (100%) and vancomycin (100%). Streptococcus haemolyticus was resistant to amoxicillin+clavulanic acid (85.71%) and ampicillin (100%) and susceptible to linezolid (100%) and rifampin (100%). Streptococcus epidermidis was resistant to amoxicillin+clavulanic acid (82.35%), ampicillin (100%), penicillin (100%) and susceptible to linezolid (91.18%) and rifampin (88.24%). Streptococcus aureus was resistant to amoxicillin+clavulanic acid (95%) and ampicillin+sulbactam (90%), and susceptible to linezolid (90%) and synercid (95%). Pseudomonas aeruginosa was resistant to amikacin (100%), meropenem (100%) and tobramycin (90%).
Conclusion
This study offers some useful information to doctors in the Mekong Delta and across Vietnam. It can be used as a good orientation in choosing the most appropriate antibiotics for treating patients with chronic rhinosinusitis. It is important to be conscious of the current trend of the bacteriological profiles and to regulate the antibiotic treatment regime to improve the effectiveness and reduce antibiotic resistance rate.
1. INTRODUCTION
Chronic rhinosinusitis (CRS) is a common chronic disease and an important health issue that affects 5-12% of the general population and has a huge impact on quality of life and productivity. It is a multifactorial condition where the microbiota plays a pathogenic role [1-3]. The use of antibiotics in CRS is currently of great interest, and novel strategies have been developed recently. However, the inappropriate use of antibiotics in clinical practice and management of CRS leads to disproportionate medical expenditure, unexpected adverse effects, and drug-resistant bacterial infections [4]. Inappropriate antibiotic treatment can change the structure of the natural commensal bacterial community and destabilize the indigenous microbiota [5]. In 2019, the World Health Organization (WHO) identified antimicrobial resistance (AMR) as one of the top ten threats to global health due to its significant impact on human health. The inappropriate use of antibiotics is widely considered the primary cause of bacterial resistance to these drugs. In developed countries, such as the USA and Canada, it is estimated that 30–50% of antibiotic prescriptions are inappropriate [6, 7]. Approximately 50% of all antibiotic prescriptions target treating upper respiratory infections, especially rhinosinusitis, suppurative acute otitis media, and acute pharyngotonsillitis. Across all conditions, an estimated 30% of outpatient oral antibiotics prescribed may be inappropriate [8]. Given the high prevalence of CRS and the variability in prescribing, overuse of unsuitable antibiotics may represent a public health threat through selective pressure on bacteria and resistance [9]. It is urgent to reduce the alarming levels of antibiotic resistance and its detrimental consequences for patients, the healthcare system, and the general population. In Vietnam, the treatment of rhinosinusitis is performed by ENT doctors, pediatricians, and family doctors. Besides that, many patients are doing self-treatment by buying drugs (including antibiotics) at drugstores. Therefore, in many patients with acute rhinosinusitis, the disease can easily turn to CRS because of inappropriate treatment. The emergence of antibiotic-resistant bacteria isolated from patients with CRS poses a significant clinical challenge, prompting increased research efforts. This study aimed to evaluate the results of bacterial cultures and antibiograms to assess antibiotic resistance patterns in prevalent bacterial species isolated from patients with CRS at Can Tho University of Medicine and Pharmacy Hospital.
2. MATERIALS AND METHODS
2.1. Study Design
A cross-sectional study was conducted on 113 patients diagnosed with CRS according to the European Position Paper on Rhinosinusitis 2020 (EPOS 2020) criteria [1]. The study was performed at the Otorhinolaryngology Department of Can Tho University of Medicine and Pharmacy Hospital between 2022 and 2023. The participants were selected using a convenience sampling method and agreed to participate in the study. All samplings were taken from patients of provinces or cities in the Mekong Delta, such as Cantho, Angiang, Kiengiang. A detailed clinical history, including age, gender, duration of discharge, and previous antibiotic therapy, was obtained. The data were collected during the consultation and from the patient’s medical records.
2.3. Endoscopic-guided Sampling
After completing the nasal cavity assessment and obtaining diagnostic images, purulent secretions were collected for culture and antibiotic susceptibility testing. The sites with copious pus and the darkest color were selected for sampling. The endoscopist determined the appropriate location and took the samples with a swab. The endoscope was inserted into the anterior nares superiorly, and the swab was inserted into the nasal cavity inferiorly. The swab tip was always kept ahead of the endoscope tip. Upon reaching the target site, the swab tip was allowed to touch the purulent discharge for approximately 20 seconds to allow absorption. The swab was then rotated to ensure that the discharge was evenly distributed around the tip. If necessary, the swab was rotated around the discharge site until it was completely covered. The goal was to collect as much purulent discharge as possible. The endoscope and swab were then simultaneously withdrawn, with the care of avoiding contact between the swab tip and the endoscope tip or the nasal vestibule from insertion to removal. The swab was immediately placed in a specimen container prepared by the assistant and securely capped. Patient information was immediately recorded on the specimen container. The specimen was promptly transported to the Microbiology laboratory of Can Tho University of Medicine and Pharmacy (within 2 hours of collection) along with a requisition form for identifying and establishing bacterial antibiotic profiles.
2.4. Microbiological Analysis
Samples were cultured and isolated on blood agar and MacConkey agar. The cultures were then incubated at 37°C for 18-24 hours. If bacteria grew, gram-stained colonies were selected for further analysis. These colonies underwent biological and chemical tests, followed by identification using the automated identification system (MicroScan). The autoSCAN-4 instrument uses a colorimetric optical system to read wells on the panel. Measure density color is the basis for colorimetric analysis. The colorimetric system measured light transmission when reading biochemical wells and measured light absorption, which lights up when reading the MIC wells. The wells of each panel contained antimicrobial agents at different concentrations. Wells with antimicrobial agents that inhibited organism growth were less cloudy. The device compared each test well reading with a threshold value (derived from the test well) and turbidity readings of the control wells in that panel and then determined whether each well had biological organisms chief or not. In this way, the autoSCAN-4 device determined the MIC of each antimicrobial substance. The microorganisms were identified by measuring a series of biochemicals contained in panels designed to identify gram-positive and gram-negative bacteria. The panels contained biochemicals that reacted with microorganisms. These reactions could be identified by the well-changing color due to pH changes, either due to the addition of reagents or due to some wells possessing or not growing organisms. The optical system incorporated a light-sensitive photodiode array to detect the amount of outgoing light through each well of the test panel. The optical system measured turbidity or discoloration in wells for organism identification and MIC determination. Each photodiode generated an electronic signal corresponding to the amount of light detected.
2.5. Results of Antimicrobial Susceptibility Testing
Antimicrobial susceptibility testing was performed on bacteria grown. The results were reported for each antibiotic tested, with one of three possible outcomes: (S) – Susceptible; (R) – Resistant; (I) – Intermediate (mainly). All relevant information was analyzed using SPSS version 22.0.
3. RESULTS
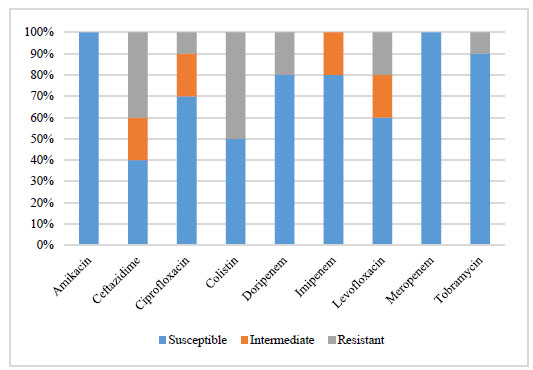
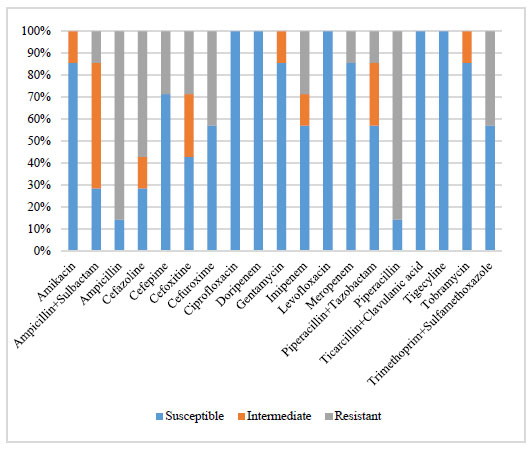
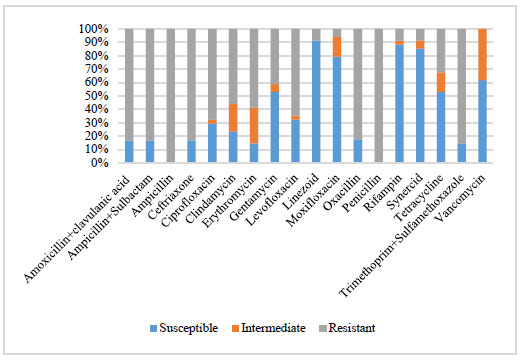
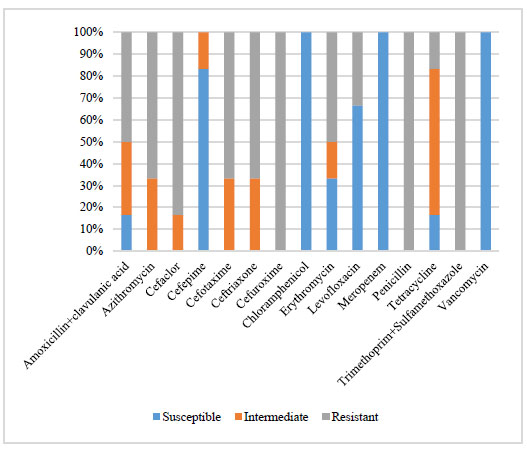
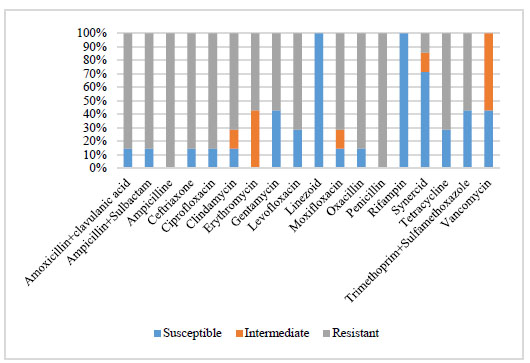
Table 1 shows that the average age of patients in the study was 46.2 years old, of which 54% were male and 46% female. Fig. (1) shows the proportion of patients who knew their accompanying medical diseases. The duration of disease <12 months accounted for 76.1%, as shown in Table 2. The culture location in the right middle nasal meatus was 58.4%, and the left middle nasal meatus was 41.6%, as displayed in Table 3. Table 4 displays the microbiological profiles. In 113 nasal swab samples, the bacteria growth was 110 (97.3%), and the number of 2 species growing on the sample was 6 (5%). In a total of 116 samples, gram-positive bacteria were more common, accounting for 75%, and gram-negative bacteria accounted for 25%. Fig. (2) shows that there were six identified common bacterial species in this study. S. epidermidis was the most frequently cultured species, accounting for 29.3% of isolates, followed by S. aureus (17.2%), P. aeruginosa (8.6%), K. pneumoniae and S. haemolyticus (6.0% each), and S. pneumoniae (5.2%). S. epidermidis was highly susceptible to linezolid (91.2%) and rifampin (88.2%) and completely resistant to ampicillin and penicillin (Fig. 3). S. aureus was highly susceptible to Synercid (95%) and linezolid (90%) and highly resistant to amoxicillin+clavulanic acid (95%), ceftriaxone (85%), oxacillin (85%) (Fig. 4). P. aeruginosa was highly susceptible to the antibiotics amikacin (100%), meropenem (100%), and tobramycin (90%) (Fig. 5). K. pneumoniae was completely susceptible to ciprofloxacin, doripenem, ticarcillin+clavulanic acid, and tigecycline (Fig. 6). S. haemolyticus was completely susceptible to linezolid and rifampin and completely resistant to ampicillin and penicillin (Fig. 7). S. pneumoniae was completely susceptible to chloramphenicol, meropenem, and vancomycin and completely resistant to cefuroxime, penicillin, trimethoprim + sulfamethoxazole (Fig. 8). Chloramphenicol, daptomycin, and tigecycline were also susceptible to 100% of test samples (Fig. 9).
| Characteristics | Age (Medium: 46.2 yrs) | Sex | ||||
|---|---|---|---|---|---|---|
| <21 | 21-40 | 41-60 | >60 | Male | Female | |
| Number (N=113) | 8 | 36 | 42 | 27 | 61 | 52 |
| Percent (%) | 7.1 | 31.9 | 37.1 | 23.9 | 54 | 46 |
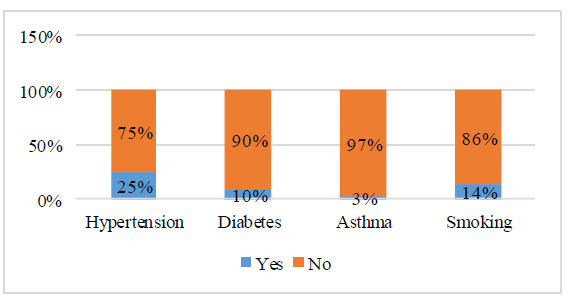
Accompanying medical characteristics (N=113).
|
Time of Disease (Medium: 8.78 months) |
Number (N=113) | Percent (%) |
|---|---|---|
| >3 - <12 months | 86 | 76.1 |
| 12-24 months | 19 | 16.8 |
| >24 months | 8 | 7.1 |
| Site of taking Samples | Right Side (N=56) | Left Side (N=57) | ||
|---|---|---|---|---|
| Number | Percent (%) | Number | Percent (%) | |
| Middle meatus | 47 | 83.9 | 49 | 86 |
| Superior meatus | 9 | 16.1 | 8 | 14 |
| Characteristics | Frequency (%) | |
|---|---|---|
| Culture results (N=113) | Growth | 110 (97.3) |
| No growth | 3 (2.7) | |
| Species growing on the sample (N=110) | 1 species | 104 (95) |
| 2 species | 6 (5) | |
| Gram bacteria (N=116) | gram-positive | 87 (75) |
| gram-negative | 29 (25) | |
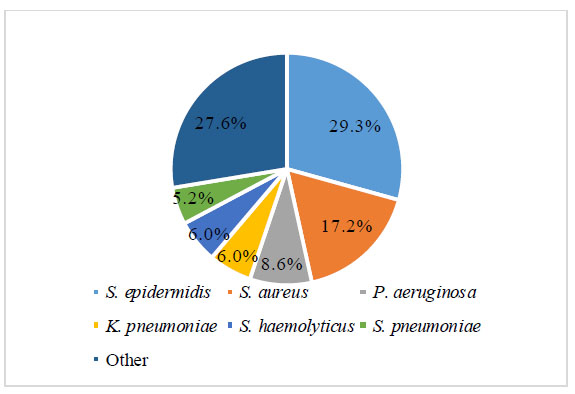
Composition of cultured bacteria.
4. DISCUSSION
The increasing rate of antimicrobial resistance is one of the most significant problems that modern medicine has been confronted with. Besides, CRS is often a poly- microbial synergistic infection and may, therefore, be harder to eradicate with narrow-spectrum antimicrobials. Continued surveillance of the patient population with CRS is essential to follow microbial resistance and susceptible patterns, to determine empiric treatment regimens with a higher probability of success, and to track growing antimicrobial resistance for public health goals [10, 11].
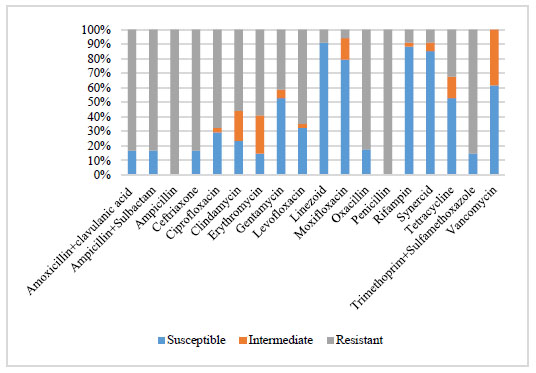
Antibiotic profile of S. epidermidis bacteria (N=34).
Antibiotic profile of S. aureus bacteria (N=20).
Antibiotic profile of P. aeruginosa bacteria (N=10).
Antibiotic profile of K. pneumoniae bacteria (N=7).
Antibiotic profile of S. haemolyticus bacteria (N=7).
Antibiotic profile of S. pneumoniae bacteria (N=6).
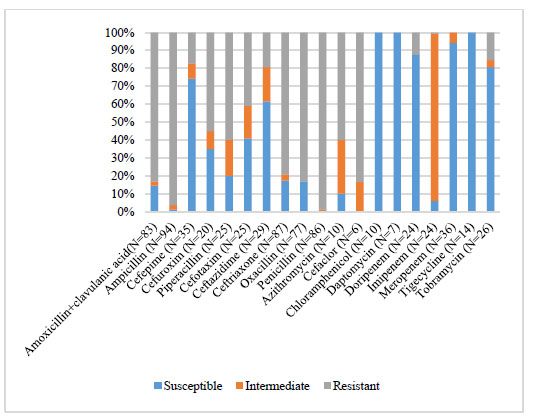
Antibiotic profile of each type of antibiotic.
Compared to the study conducted by Quyen (2020), the rate of bacterial growth in the sample was 38.4%, and in samples growing two bacterial species was 3.6% [12]. Research by Urban et al. (2020) in Hungary showed that the growth rate was 100%, with an overall rate of 2.61 species per sample [13]. This difference may be due to differences in the methodologies used for the transportation and cultivation of specimens, patient population, location, pre-study treatment status, and study duration.
The microbiology profile in our study population showed that 75% of the isolated organisms were gram-positive, which may be more common than gram-negative. In the study by Liu et al. (2020) in China, the proportion of gram-positive bacteria was also more dominant than gram-negative bacteria [14].
There were 22 cultivable bacterial species in our study, of which the Staphylococcus accounted for the highest proportion, with 10 species (45.5%). The comprehensive study by Okifo O (2022) showed that Staphylococcus accounts for the majority of the proportion, and in the study by Lucas et al. (2021), Staphylococcus also accounted for 50% [15, 16].
There were six major bacteria isolated. Among them, S. epidermidis was the most common bacteria (29.3%), followed by S. aureus accounting for 17.2%, and P. aeruginosa accounting for 8.6%. Further, K. pneumoniae and S. haemolyticus accounted for 6.0%, and S. pneumoniae accounted for 5.2%. This is quite similar to Brook’s review (2016), which showed predomination by S. aureus, S. epidermidis, and anaerobic gram-negative bacteria [11]. Additionally, other bacteria were isolated, including E. cloacae, S. warneri, C. fameri, and S. maltophilia, but in very few cases.
S. aureus showed high susceptibility to synercid (95%) and linezolid (90%) and high resistance to amoxicillin+ clavulanic acid (95%), ceftriaxone (85%), and oxacillin (85%), respectively. Research by Hoa (2016) also showed that the multiresistance of S. aureus was high. Specifically, regarding antibiotics, penicillin, cefotaxime, erythromycin, clindamycin, moxifloxacin, and co-tri- moxazole had resistance rates of 90.9%, 63.6%, 45.4%, 36.4%, 18.2%, and 36.4% [17]. The study of Bhattacharyya et al. (2015) about trends in antimicrobial resistance in 392 culture samples of CRS showed that S. aureus was the most commonly isolated organism (19.0%). They also revealed that S. aureus remains a significant pathogen in approximately one-fifth of cases of culture-positive CRS and commonly exhibits multidrug resistance [10]. The above results demonstrated that the multi-antibiotic resistance trend of S. aureus is common.
P. aeruginosa showed 100% susceptibility to amikacin and meropenem (100%), 90% to tobramycin, and a relatively low rate of multi-resistance; the highest was found to be 50% to colistin and 40% to ceftazidime, and aztreonam was 30% in our study. Compared to the study of Hoa (2023), P. aeruginosa had the highest resistance to ofloxacin at 63.6% [18]. The research by Hoa (2016) showed that P. aeruginosa was 100% susceptible to gentamycin, tobramycin, amikacin, and ciprofloxacin [17]. Research by Quyen (2020) also showed that S. aureus was 100% susceptible to gentamycin, ceftazidime, amikacin, levofloxacin, imipenem, and meropenem [12]. The above results indicated that P. aeruginosa was still susceptible to many antibiotics, but it was also resistant to some antibiotics.
K. pneumoniae was completely susceptible to ciprofloxacin, doripenem, ticarcillin + clavulanic acid, and tigercyline. Research by Tru (2022) showed that K. pneumoniae was susceptible to cefepime 49.4%, imipenem 56.1%, ertapenem 57.6%, levofloxacin 14.2%, and ciprofloxacin 15.2% [19]. Research by Trang (2023) also concluded that K. pneumoniae was highly resistant to many groups of antibiotics [20]. It shows that you should do an antibiotic test if you suspect it is K. pneumoniae because it is difficult to predict which antibiotic K. pneumoniae will respond to the most when treated empirically.
S. haemolyticus in our study was completely susceptible to linezolid and rifampin and completely resistant to ampicillin, penicillin, and multi-resistant to many antibiotics, of which the highest rate was ciprofloxacin with a rate of up to 85.7%, levofloxacin 71.4%, oxacillin 71.4%, cefoxitin 71.4%, clindamycin 57.1%, erythromycin 57.1%, and gentamycin 57.1%.
In this study, S. pneumoniae was completely susceptible to chloramphenicol, meropenem, and vancomycin and completely resistant to cefuroxime, penicillin, and trimethoprim + sulfamethoxazole. Compared to the study of Quyen (2020), S. pneumoniae was still 100% susceptible to chloramphenicol and 100% resistant to erythromycin and clindamycin [12]. Research by Yen et al. (2022) showed that S. pneumoniae resistance to erythromycin and clindamycin was 84.2% and 67.3%, respectively, with no vancomycin-resistant samples (0.0%) [21]. Research by Son et al. (2022) in Nghe An (North of Vietnam) showed that S. pneumoniae was resistant to >90% of macrolides, trimethoprim + sulfamethoxazole and there were no cases of resistance to vancomycin or linezolid [22]. Comprehensive research by Soa et al. (2022) also showed that S. pneumoniae had a high resistance rate to macrolides, penicillins, and sulfamides and a highly susceptible rate to vancomycin or linezolid [23]. This shows that S. pneumoniae is still susceptible to vancomycin.
4.1. The Resistance of Bacteria to many kinds of Antibiotics
Amoxicillin + clavulanic acid was resisted and intermediated by 83.1% of the bacterial species in our study. In the research by Yen (2022), the resistance rate to amoxicillin + clavulanic acid was 66.9% [21], and it was 25% in Quyen’s study (2020) [12]. The above ratios showed that amoxicillin + clavulanic acid had an increasing resistance rate over time.
Cefepime still showed an 83.3% susceptibility rate with 16.7% resistance as per this study’s bacterial species. In Yen's study (2022), the cefepime resistance rate of gram-positive bacteria was 20.6%, and gram-negative bacteria was 79.4% [21]. These results were different, which can be explained by the fact that cefepime was resistant mainly to gram-negative bacteria. Our sample had a low percentage of gram-negative bacteria, so the overall resistance rate was lower.
Ceftriaxone was resisted by 66.7% bacterial species culture in our study. Research by Quyen (2020) showed that ceftriaxone had a rate of 59% susceptibility and 33.3% resistance [12]. This rate showed that ceftriaxone has rapidly increased resistance recently.
Cefuroxime was resisted by 100% bacterial species. Cefuroxime is almost a popular first-line antibiotic in the empirical treatment of rhinosinusitis. With the low susceptibility as shown by the study results, we need to consider when to use cefuroxime as the first-line empirical antibiotic treatment.
Levofloxacin remained susceptible at 66.7% and resistant at 33.3% of bacterial cultures in this study. Research by Yen (2022) also had quite similar results to ours. Specifically, levofloxacin was resistant to 57% of gram-positive bacteria and 43% of gram-negative bacteria [21].
In our study, penicillin was resisted by 100% bacterial species. Research by Yen (2022) showed that the resistance rate to penicillin of gram-positive bacteria was 9.2% and gram-negative bacteria was 83.8% [21], and research by Hoa (2016) had a penicillin resistance rate of 90.9% [17]. The three studies above lasted for 7 years (2016-2023), thereby showing that penicillin has long been highly resisted by many bacterial species.
In our study, vancomycin showed 100% susceptibility. However, the research by Yen (2022) found the emerging resistance to vancomycin among certain bacteria [21]. Especially 10.4% of S. aureus and 16.5% of Staphylococcus spp. exhibited resistance, and notably, the study did not report any vancomycin resistance in S. pneumoniae isolates. While vancomycin and carbapenems often require careful consideration before use due to potential resistance concerns, their effectiveness in treating seriously ill patients necessitates continued use, so resistance is difficult to avoid.
These results indicate the importance of selecting the appropriate antibiotic therapy when treating CRS to avoid antibiotic resistance and also as a warning to consider how sinusitis responds to antimicrobial therapy, particularly when antibiotic resistance is still rising. Numerous investigations have demonstrated that treating bacterial sinusitis with antibiotics too early or unnecessarily does not prevent the complications. Furthermore, studies established that the use of antibiotics affected the variety of normal microbiota composition and promoted the dominance of antibiotic-resistant species [24].
We mainly compared our results with local research because of the similarities in the regions and the differences in antibiotic resistance between areas. Our study has a limitation because of the number of samplings, and it was only conducted in one institute; thus, it requires more studies with more institutes.
CONCLUSION
The bacterial culture results and antibiograms in our study showed that the gram-positive bacteria were more common. In 22 cultivable bacterial species, six major microorganisms were isolated, and S. epidermidis was the most common bacteria (29.3%). The multi-antibiotic resistance trend of S. aureus was common. Further, P. aeruginosa was still susceptible to many antibiotics, and S. pneumoniae was susceptible to vancomycin. Regarding the resistance rate of bacteria, amoxicillin+clavulanic acid had increased resistance over time, cefuroxime was 100% resistant, and penicillin was 100% resistant. It is important to be conscious of the current trend of the bacterial profiles and to adjust the antibiotic regime to improve the quality of treatment, thereby saving money. Nonetheless, the most crucial thing is to reduce the antibiotic resistance rate.
AUTHORS' CONTRIBUTION
It is hereby acknowledged that all authors have accepted responsibility for the manuscript's content and consented to its submission. They have meticulously reviewed all results and unanimously approved the final version of the manuscript.
LIST OF ABBREVIATIONS
| CRS | = Chronic Rhinosinusitis |
| ENT | = Ear Nose Throat |
| WHO | = World Health Organization |
| AMR | = Antimicrobial Resistance |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The research was accepted by the Ethics and Review Board Can Tho University of Medicine and Pharmacy, Vietnam (approbations 22.109.HV/PCT.HĐĐĐ-ĐHYD).
HUMAN AND ANIMAL RIGHTS
All procedures performed in studies involving human participants were in accordance with the ethical standards of institutional and/or research committees and with the 1975 Declaration of Helsinki, as revised in 2013.


