All published articles of this journal are available on ScienceDirect.
Successful Reduction of Blood Culture Contamination in an Emergency Department by Monitoring and Feedback
Abstract
Background:
Blood Culture (BC) contamination is a common problem in the Emergency Department (ED) and is associated with prolonged length of patient stay and excess costs.
Objective:
The study aimed to investigate the impact of monthly monitoring and feedback of BC results on contamination rates.
Methods:
Data from a previous study showed that the contamination rate in the ED consistently exceeded the recommended level. This triggered an ad hoc Quality Improvement team to develop and implement a corrective action plan. In 2017, BC contamination rates were reported to the ED on a monthly basis. In response to this, ED staff conducted intensified educational workshops, followed by private counselling and competency assessment of nurses who collected contaminated BCs.
Results:
A total of 12 educational workshops were conducted in February and March, 2017. The intervention resulted in >60% reduction in the contamination rate, from 8.6% baseline level to less than 3%. Of the 2660 BC sets drawn in 2017 from 1318 patients, 128 (4.8%) were contaminated, accounting for 39.5% of the total number of positive cultures. Sixty percent of the contaminated BCs grew Coagulase-negative Staphylococcus species; other contaminants included Corynebacterium spp., Micrococcus spp., Propionibacterium spp., viridans Streptococcus, and Neisseria spp.
Conclusion:
Continuous monitoring and feedback of contamination rates reduced BC contamination.
1. INTRODUCTION
Blood Cultures (BCs) are an essential diagnostic tool for the detection of bacteremia and fungemia and are required to guide specific antimicrobial therapy in septic patients. BCs are commonly performed in the Emergency Department (ED); however, contaminated BCs (i.e., false-positive BCs) are a common problem and represent up to half of all positive BCs [1, 2]. Indeed, false-positive BCs due to specimen contamination with skin bacteria range from 0.6% to over 6% and associated with unnecessary exposure to antimicrobials and their associated toxicity, additional cultures and other diagnostic tests, and prolonged hospital stays [1, 5-7]. Contaminated BCs increase laboratory costs by approximately 20%, are associated with a nearly 40% increase in antibiotic charges, and as much as 5 additional days in the hospital [1, 8-10]. Several techniques have been used to reduce BC contamination including the use of specific disinfection materials [2, 11], educational interventions [2, 6, 12, 13], collection from separate venipuncture sites [5, 7], use of the outmoded double-needle technique [7], commercial BC kits [3, 14, 15], and reliance on specially trained staff or dedicated phlebotomy teams [2, 7, 8, 16]. The aims of the present study were to assess BC contamination in the ED and the impact of monthly monitoring of BC contamination and feedback on contamination rate.
2. MATERIALS AND METHODS
2.1. Study Setting
The present work was carried out as a quality improvement project, part of the hospital’s clinical services and quality management program, and therefore, ethical approval was not required. The study was conducted at Qatif Central Hospital, a 335-bed district general hospital serving a population of more than 500,000. The project was registered with and approved by the hospital’s Quality and Patient’s Safety department. The hospital provides all general medical and surgical services; supports a range of outpatient facilities; and acts as a center for the coordination of health services provision throughout a defined geographical area in the Eastern Province of Saudi Arabia. In addition, the hospital is situated on a busy highway between two industrial cities, providing care for road traffic accidents victims. The 64-bed ED with an average of 250,000 annual visits includes the following services: triage (3 beds); medical assessment (18 beds); surgical assessment (10 beds); obstetrics/gynecology (3 beds and 1 delivery room); observation (16 beds); pediatrics (7 beds); and resuscitation (4 rooms for adult and 2 for children). The isolation facilities include one side room and one negative pressure room. There were 107 practicing nurses during the study period. Guidance on appropriate BC collection protocols was provided by the clinical microbiology laboratory. Nurse staff members performed all phlebotomy.
2.2. Blood Culture Processing
The microbiology laboratory within the hospital recommends that blood for cultures is drawn using an aseptic technique. The venipuncture site is to be disinfected with 2% w/v chlorhexidine gluconate in 70% isopropyl alcohol and, when these are not available, 70% isopropyl alcohol followed by 10% povidone iodine is used. The guidance recommends disinfecting the venipuncture site in concentric circles beginning at the center of the site, allowing a minimum of 1.5 minutes application time before drawing the blood culture. The septum of the BC bottles is disinfected with 70% isopropyl alcohol. The standard for routine BCs is a minimum of two sets (three sets for suspected infective endocarditis) drawn from different peripheral venous sites in order to optimize the recovery of organisms and to assist in the determination of the clinical significance of certain isolate(s). It is a standard practice to collect one set from the peripheral line and the other set from the central line for patients with a central venous catheter. Blood drawn from a single venipuncture is regarded as a single set regardless of how many BC bottles were inoculated; routinely, this includes an aerobic and an anaerobic bottle for adults, with or without resins depending on whether the patient is receiving antibiotics. The BACTECTM 9240 BC system (Becton-Dickinson, Riyadh, Saudi Arabia) is used for all BCs. Each BC is incubated for 5 days before considered negative. Cultures from patients with suspected endocarditis, heart lesions, or prosthesis or from patients suspected to have brucellosis are incubated for 21 days. When bacterial growth is detected in a BC bottle, an aliquot of broth is gram-stained and subcultured. All positive gram stain results are conveyed the same day to the ward, as well as preliminary and definitive identification and antimicrobial susceptibility result when they become available.
2.3. Definition of Contamination
The following criteria for differentiating likely true bacteremia from contamination were used: (1) identity of the organism, (2) number of different organisms cultured, (3) number of positive BC sets, (4) number of positive BC bottles within a BC set, (5) time to growth, and (6) source of cultures (catheter drawn vs. percutaneous) [3, 9]. Samples were considered to be contaminated if common skin bacteria (Corynebacterium spp., Bacillus spp., Propionibacterium spp., viridans streptococci, Micrococcus spp., coagulase-negative Staphylococcus spp. [CoNS]) were cultured in only one of a series of BCs [7]. In addition, BCs were defined as contaminated if multiple BC sets were positive with different species or the antibiotic susceptibility patterns for the isolates were different, and the results of the BC were not compatible with the clinical condition of the patient. Polymicrobial cultures with more than one contaminant species were counted as a single contaminated BC [14]. Other clinical and laboratory clues were used to predict likely true bacteremia, including fever or hypothermia (and other signs of sepsis), leukocytosis or leukopenia, hypotension, or high C-Reactive Protein (CRP) levels [3, 15]. The contamination rate was determined by dividing the number of contaminated cultures by the total number of cultures collected.
2.4. Intervention
Beginning in February 2017, charts with monthly contamination rates were reported to the head nurse and the director of the ED, along with copies to the Quality and Patient’s Safety department, Infection Control section, and chief nurse in the hospital. The microbiology laboratory provided the ED with guidance on evidence-based recommendations for appropriate BC collection techniques. Additionally, in response to the initial high contamination rate, the staff in the ED conducted a series of workshops to educate the nurses involved in BC collection. These workshops were intensive in February and March to cover most nurses involved in BC draw, and included a lecture presentation, short video, and demonstration on the collection protocol. The lecture presentation started with clinical scenarios of consequences of BC contamination, followed by a summary of adverse outcomes and detailed instruction on how to conduct BC collection aseptically. The 5-minute locally produced video covered all aspects of the aseptic technique using the BD Vacutainer® system. Each workshop ended with a demonstration of the materials used to collect blood for culture and questions handling. In addition, the ED clinical instructor conducted bedside discussion and explanation of the BC collection protocol. With the help of MedicaPlusTM Hospital Information System (Riyadh, Saudi Arabia), it was possible to compile data regarding the individuals collecting the BCs, the time at which the specimens were taken, and when these specimens were received in the laboratory. As a supportive measure, the patients who had contaminated BCs were identified and the names of nurses who collected contaminated BCs were given to the ED. These nurses were counselled privately and reassessed for competency on the appropriate aseptic technique. Staff nurses identified with more than two contaminated BC episodes were asked to be involved in the educational workshops by giving presentations to their peers, and the private counselling continued as necessary.
3. RESULTS
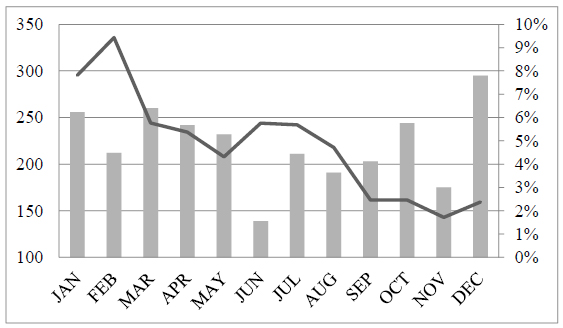
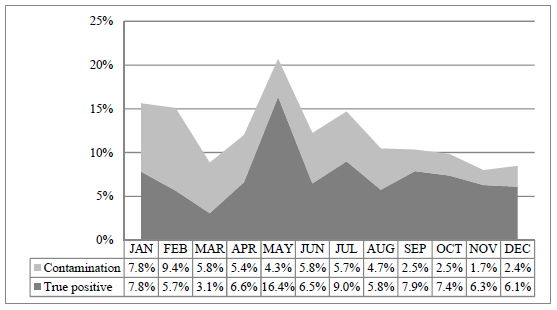
The contamination rate of BCs in January 2017 before the intervention started was 7.8%. In response, 12 workshops were conducted in February and March, with an average attendance of 5 to 10 staff nurses and students. These workshops were initially offered to nurses on duty in the morning and afternoon and, in March, very early morning sessions were also offered to those working in the night shift. After covering 90% of staff involved in BC collection, workshops were offered as needed to new staff nurses or those who collected more than two contaminated BCs. The intervention led to a decrease in contamination from 9.4% in February to 2.4% in December Fig. (1). The overall trend of contamination showed a decrease during the project period, apart from a slight increase in the summer (likely due to shortage of staff during vacations season), to a sustainable level below 3%. Results of all BCs collected during the study period are presented in Table 1 and Fig. (2). Half of the positive BCs in January and 62.3% in February were contaminated; in contrast, 24.0%, 25.3%, 21.3% and 28.2% in September, October, November and December, respectively were contaminated. This represents a consistent improvement in the predictive value that a positive culture is significant.
The most common microorganisms and contaminants recovered from BCs during the study are shown in Table 2 and 3, respectively. CoNS, Escherichia coli, and Staphylococcus aureus represented 52.1% of all BC isolates. When the total positive BCs were analyzed for contaminants, 60.9% were CoNS. More than one bacterial species was present in 10 of 324 positive BCs (3.1%) and at least one bacterial contaminant was recovered from the majority (82%) of the mixed cultures.
| Blood Cultures | No. (%) | No. of Patients (%) |
|---|---|---|
| Positive cultures • Likely to be true bacteremia • Likely to be contamination |
324 (12.2) 196 (7.4) 128 (4.8) |
264 (20.1) 152 (11.5) 112 (8.5) |
| Negative cultures | 2336 (87.8) | 1054 (80) |
| Total | 2660 | 1318 |
| Organism | No. (%) of Isolates |
|---|---|
| CoNS | 95 (29.3) |
| Escherichia coli | 38 (11.7) |
| Staphylococcus aureus | 36 (11.1) |
| Klebsiella pneumoniae | 21 (6.5) |
| Brucella spp. | 14 (4.3) |
| Streptococcus pneumoniae | 12 (3.7) |
| Salmonella spp. | 10 (3.1) |
| Corynebacterium spp. (other than C. jeikeum) | 10 (3.1) |
| Micrococcus spp. | 8 (2.5) |
| Proteus mirabilis | 7 (2.2) |
| Organism | No. (%) of Isolates |
|---|---|
| CoNS | 78 (60.9) |
| Corynebacterium spp. (other than C. jeikeum) | 10 (7.8) |
| Positive cultures with inconsistent organism type | 10 (7.8) |
| Others | 9 (7.1) |
| Micrococcus spp. | 8 (6.25) |
| Propionibacterium spp. | 5 (3.9) |
| Viridans group Streptococci | 5 (3.9) |
| Neisseria spp. | 3 (2.3) |
| Total | 128 |
4. DISCUSSION
Bloodstream infections are a serious medical condition, associated with significant morbidity and mortality. The latter varies between 14% and 34%, depending on whether the infection originates in the community or the hospital [17, 18]. Early administration of appropriate antimicrobial agents directly influences the patient outcomes [19] and BCs are needed for organism identification and susceptibility testing to guide the selection of specific, appropriate antimicrobials. However, the value of BC is related directly to the incidence of false-positive results. In many EDs, BC collection frequently occurs without attention to a standardized process for specimen collection [20]. Although it is recommended that target rates for BC contamination should not exceed 3% [4], the contamination rate in many institutions actually exceeds 7% [1, 8, 14] with the highest rates found in ED settings [6, 20-22]. In our institution, 7.8% of the total BCs collected from ED in January 2017 were contaminated. This triggered an ad hoc quality improvement team to develop and implement a corrective action plan to improve the standard of BC collection technique. The cause of high ED contamination rates was likely multifactorial, including frequent staff turn-over, fast-paced working environments, and the time pressure of collecting specimens before administering an initial dose of antibiotics or the need to intervene in the management of other patients while collecting BCs [6, 20-22]. While adherence to evidence-based best practice when collecting BCs is supposed to be the standard of care, compliance can be unsatisfactory and the high BC contamination rate might be a result of the lack of training and education, lack of surveillance and monitoring, inadequate staffing, shortage of materials, or the use of poor quality materials [7]. From previously published work, hospital-wide educational intervention had led to reductions in contamination rates at our institution, but rates for the ED remained high due to lack of attendance [13]. Because our hospital did not invest in the establishment of a dedicated phlebotomy team for BC collection, the present study investigated the effect of detailed monitoring and monthly feedback on contamination rate. During educational sessions, it was found that some of the nurses were not aware of the existence of the BC collection protocol. Although nurses in the ED are busy with their clinical work by nature, it must be emphasized that appropriately collected BC will lead to less contamination and therefore less work, due to unnecessary admissions, antibiotic use, and repeat of laboratory investigations. Gibb et al. found that monitoring and feedback of the incidence of contamination were successful in achieving a 50% reduction, although the rate of contamination in BCs collected by nonphlebotomists did not change [23]. The present study showed a 75.6% reduction in contamination rate, comparing data from January and February (av. 8.6%) before the start of intervention to data from November and December (av. 2.1%). While it is not new to show that monitoring of BC results and feedback reduces the contamination rate, the present study led to the assessment of staff competency in drawing blood for cultures, availability of a clear protocol or policy, currently used practices, contamination rates, and the effect of educating staff nurses regarding the contamination rate. This is the first study showing successful reduction of BC contamination in the ED where all BCs were collected by nurses and not by a phlebotomy team.
Clinicians often respond to these false-positive tests by initiating diagnostic studies and treatments that would otherwise not have been pursued. Two studies estimated that BC contaminants were associated with increased length of hospital stay, by 1 day and 3 days, and additional hospital charges, by $8,720 and $8,750 per patient, respectively [8, 24]. A similar case-control study showed statistically significant differences between false positive and true negative results in the mean length of hospital stay (5.4 days) and total costs ($7,502) [10]. If we take the average contamination rate in January and February as a representative rate before the start of the project, we can compare the cost of contamination with and without the intervention. By using the estimated cost of $8000 per false positive BC, the difference in hospital costs in our institution during a 12-month period assuming no intervention (8.6% contamination rate [January-February]) and the same period with the effect of the current project (2.1% contamination rate [November-December]) is approximately $1,384,000 ($1,824,000 vs. $440,000). While educational interventions lead to reduction in BC contamination, maintaining acceptable contamination rates can be quite challenging. A recent review suggests that venipuncture and the use of phlebotomy teams are effective for reducing BC contamination rates and are recommended as evidence-based “best practice” [25]. In addition, several studies support that phlebotomy teams are not only cost-effective but also cost-saving solely based on reduced BC contamination, driven by reduced hospital length of stay, pharmacy and laboratory services [2, 8, 16, 21]. The estimated savings per year achieved by the current project would counterbalance the cost of adoption of a phlebotomy team.
Limitations in this quality improvement project included the lack of a control group. No attempts were made to determine neither the number of admissions, patient’s call back, diagnostic investigations nor antibiotic use among patients with contaminated BCs. Although it was possible to reduce the contamination rates to acceptable levels, it is harder to maintain the competency of a large number of healthcare workers, which requires continuous follow-up interventions. Because nurses are understaffed and extremely busy with their clinical responsibilities, they are unlikely to be able to comply consistently with the recommended best practice BC collection protocol.
CONCLUSION
In conclusion, the increase in patient morbidity and excess costs caused by false-positive BC supports the use of substantial efforts to decrease the rate of contamination. While the current project aimed at examining education of the ED nurses on proper performance of BC collection procedures, there are difficulties in achieving long-term sustainable low contamination rate, and the utilization of a dedicated phlebotomy team may likely be more effective and easy to follow.
DISCLOSURE
This study was presented on the American Society for Microbiology (ASM Microbe), 2017 at New Orleans/USA, abstract no. 2017-A-4494-MICROBE.
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
The project was registered with and approved by the hospital’s Quality and Patients’ Safety department and reference number is QCH-LAB-2017-03.
HUMAN AND ANIMAL RIGHTS
No animals/humans were used in the study that are the basis of this research.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
The author confirms that the data supporting the findings of this research are available within the article.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
I gratefully acknowledge Dr. Patrick Murray for editing the manuscript and his valuable comments. I thank Ms. Maha Al-Ibrahim and Mr. Jaffar Altowaileb for calculating the contamination rate. I also thank Mr. Ali Alismael, Mr. Mohammed Bazroon, Ms. Mona Alfareed, Ms. Zahra Taleb, Dr. Raafat Alosta and Ms. Fadhila Alobaidan for their efforts with the educational activities.


